The operating room (OR) is like a living center. It runs around the clock with several moving parts and people. Every detail matters at every point of service – from pre-operative procedures, surgery scheduling and supply planning to room set-up, equipment cleaning and patient discharges.
Despite its revolving activity and potential for errors, the OR is expected to perform and transition smoothly and expediently, in order to best meet the needs of patient care and hospital budgets.
“Studies show astronomical OR costs per minute. Any time you can shorten the turnover time turns that non-revenue generating time into revenue generating time; that adds value for everybody. Any product or service that supports the efficiency of the OR to meet the demand of scheduled starts has value directly to the bottom line of a hospital,” explains Suzanne Champion RN, BSN, MBA, CNOR, Director Clinical Operations, U.S. Acute Sales, Cardinal Health.
In this article, industry representatives discuss the challenges of OR scheduling and turnover and the technology and supplies that help improve efficiency with communication, workflow and throughput, as well as help achieve better patient and staff satisfaction and financial standing.
Scheduling snafus and solutions
Older processes may impede scheduling and turnover, Walsh noted. “Mostly there are broken processes that have simply been grandfathered in. Hospitals, and more specifically ORs, need more sophisticated tools than simply implementing EHRs. ORs need more efficient communication with physician offices, and they need to embed the institutional knowledge of the scheduling process into lean processes optimized with better math to ultimately yield increased efficiencies that include turnover, scheduling and total volume.”
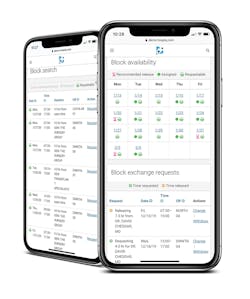
She pointed to the LeanTaaS iQueue for OR suite to timely communicate scheduling information to the team. “The iQueue aims at increasing access to ORs through better scheduling, increasing accountability with how block time is monitored and repurposed, as well as increasing visibility into what the data is telling us – pushing data automatically through mobile and web to all users (surgeons, administrators, etc.), so that everyone can have more data-driven conversations that are backed with trustworthy data. For those that want raw data and the ability to slice and dice on their own, that can be accomplished, but for the older surgeons who are not as mobile/internet savvy, we push information directly to them, which can be viewed through a simple text message with easy-to-understand visuals.”
The suite has saved both time and money, she added. “Our tools will allow physician offices to schedule surgeries sooner so that the patient wait time is less. There is tremendous value in increasing efficiencies and doing more in their business hours. The median prime time utilization increase for our customers that have been live for a year or greater is 6%. Doing even 1% more volume means a very significant financial return when it comes to revenue in the OR! In general, the most consistent feedback we hear is how much iQueue has enhanced the scheduling process for cases done outside of block time (this is roughly 35-50% of all cases) for the OR scheduling team as well as the physician offices’ scheduling team(s). In addition, we hear that iQueue helped create a single source of truth for reporting metrics.”
Multiple individuals with different responsibilities in different locations trying to coordinate the surgical journey can break down scheduling, states Jeff Robbins, LiveData Founder and CEO. “Surgical scheduling is inherently complex. It reaches beyond the simple surgical appointment slot to include patient pre-operative tasks, prepping the patient on the day of surgery, and often includes follow-up actions. Scheduling access is also not confined within the hospital walls. Patients with their family members, along with nurses, anesthesiologists and surgeons (who are often not employed by the hospital) need access and input to surgery schedules.”
An absence of up-to-date information can disrupt scheduling and attendance, Robbins affirmed. “The inability to share real-time information across the community of individuals involved in a patient’s entire surgical journey contributes to inefficiencies in surgical scheduling. Another challenge is that surgery requires patients to complete a list of pre-operative tasks to ensure surgical readiness. A lack of real-time status on progress against this list can cause last-minute cancellations. Giving everyone involved in the surgical process appropriate access to the information they need, no matter where they are, eliminates issues like patients arriving for surgery with incomplete pre-operative tasks, thus forcing the cancellation of surgery. For the OR team, being able to see the status of a patient in the perioperative process helps them move patients through the surgical preparation process and keep the surgeries moving on time.”
He recommended the LiveData PeriOp Manager suite to track activities in real time. “LiveData PeriOp Manager provides real-time situational awareness to optimize the perioperative experience for patients, their families, clinicians, and the OR support team. It simplifies scheduling, provides real-time data on patient progress through milestones, and gathers data to help streamline workflows. Interactive tools enable a personalized pre-surgery workup to be created for patients. Clinics, schedulers, and family caregivers can track and coordinate patient surgical readiness. The same kind of tracking and visualization is available in the pre-op area, so clinicians can make sure the patients are progressing through their preparations on the day of surgery. Hospitals can also display HIPAA-compliant patient status through the surgical process to help families better understand where their loved ones are in the surgical journey.”
The tools have increased scheduling accuracy and number of surgeries, he shared. “Customers have reported more than a 70% improvement in Firs t Case On-Time Starts, a 65% increase in case scheduling accuracy, and up to 27% decrease in cancellations all within the first six months of using LiveData’s tools. The actionable data provided by the system helps increase the number of cases that can be handled each day, allowing patients to get the surgery they need faster.”
Surgeon scheduling
Slow updates of unused time may hinder planning, Harber added, “If a surgeon knows they won’t use a specific block of time, they should release that time early, which enables other surgeons to book into it. While surgeons have the best intentions, they don’t typically release their blocks early enough for other surgeons to utilize the newly created time. Perioperative departments have implemented auto-release policies for unused time, but these typically take place 24 to 72 hours before the block time, which is not sufficient for other surgeons to claim for their cases. Predicting OR time that will not be used, prompting surgeons to release it early, and making it available for other surgeons through a marketplace-like experience removes a lot of the cumbersome and manual processes that are currently required just to understand what OR time might be available to book a patient case into.”
He suggested Hospital IQ’s Perioperative solution as a means to deliver current information and data. “Hospital IQ’s Perioperative solution helps improve OR throughput, which includes turnover time, by giving real-time visibility to the current performance of the rooms running in the OR, as well as predicting which rooms will need to be run to accommodate each day’s cases. In addition to these predictive and real-time capabilities, Hospital IQ automates the creation and distribution of tailored scorecards of key operational metrics that can be shared with all stakeholders to build consensus on the actions needed to make improvements. Our platform uses simple and clear emails to communicate actions, needs, performance, etc. Many users experience Hospital IQ via wall displays throughout the Perioperative department to understand the status of the current day’s cases, as well as overall performance of the department. In addition, it predicts which surgical blocks are most likely to go unused, giving other surgeons and schedulers the opportunity to book cases and fill those primetime slots.”
Multilevel communication can cause a lag in scheduling, acknowledge Vicki Harrison and Mark Stega, MD, Optimium Health. “Inefficient communication between surgical offices, surgical posting, and the pre-anesthesia teams at the hospital or surgi-center is the primary problem area. Most communication occurs via FAX, which often has inherent legibility and timeliness issues. Phone communication is also an issue when messages are not picked up on message machines or passed on accurately or in a timely manner.
This may slow down or halt surgeries and impact patients and costs, Harrison and Dr. Stega explained. “There can be 75-150 information exchanges that occur between a surgeon’s office, the perioperative department at the hospital or surgi-center and the patient at the primary level, and secondary information exchanges between finance/insurance, equipment, and device ordering and surgical supply and tray management. If any or several of these information exchanges is incorrect, untimely or omitted altogether, an on-time surgery is at risk. Case delays and cancellations are very stressful for patients. Reducing unnecessary changes and uncertainly will improve both patient and family caregiver satisfaction and goodwill. Staff will benefit because they will spend less time “putting out fires” due to communication errors, omissions, and untimely exchanges. Eliminating unnecessary clerical work will put staff focus on the clinical work to be done, which is what they enjoy, and what ultimately drives successful patient outcomes. And for the hospital or surgi-center, improved staff productivity will reduce the cost per patient and potentially provide incremental revenue due to improved patient throughput.”
They presented the Optimium Health OPTIMI$ER application to support integrated communication across the team. “Optimium Health’s OPTIMI$ER is a workflow assistance package that is tailored to improve the entire perioperative process from the initial surgical consultation to patient discharge and follow-up. It serves to improve the efficiency and organization of the team members involved in the process and ultimately reduces delays and cancellations, creates high OR throughput, and improves patient safety. In general, all of the OPTIMI$ER products work by utilization of electronic checklists, dashboards, business rules, and real time reports. Each served business segment implements a different set of these components that are tailored to the institution’s particular workflow.”
The system has increased workflow transparency and reduced procedure delays and cancellations, they addressed. “After implementation of our OPTIMI$ER, nursing satisfaction went from 28% to 78%.
Operational obstacles and tools
Pre-operative procedures’ completion, available staffing and supplies, multi-department communication, unexpected events and more can all affect OR timing, turnover and throughput.
ORs need to grasp a clear view of the surgical day and needs, guided Harber of Hospital IQ. “The full scope of the surgical day needs to be considered:
- The day needs to start as per the plan
- As the day progresses, the current state of operations needs to be well understood; what cases are on-track, what cases are delayed, which rooms will run longer than expected, which cases have special needs
- Having this information available in real time helps perioperative leaders ensure that they have the right resources in place when the room is ready.”
Yet, a well-intentioned plan is vulnerable to unforeseen circumstances, notes Zadeh of Leap Rail. “There are few factors that make managing ORs in general, and turnover specifically, very challenging. An OR environment is very dynamic: surgeries might take longer than anticipated, the patient might be late or have complications before/after the procedure, and unexpected events such as trauma cases can cause drastic shifts in what was planned for the day. And all of these events, and much more, occur frequently, and when you combine them all together, it’s no surprise why it’s so hard to manage resources effectively in the operating suite.”
These changes in the schedule can cause dissatisfaction among patients, families and teams. “Dealing with delays and not knowing when your loved one will be able to leave the OR are big drivers of patient satisfaction. The same is true for staff dissatisfaction and burnout. Unanticipated late nights, delays, and miscommunication contribute to staff issues and Leap Rail has been shown to improve the OR on all of these fronts.”
Zadeh called out the LeapRail OR Scheduling Decision Support platform to manage scheduling and workflow. The platform has helped raise efficiency and decrease cancellations, he shared. “Our artificial intelligence enabled system can predict how long each surgery will take 70% more accurately than the best EMRs currently used in the market. This improvement allows for everybody, from surgeons, to anesthesiologists, nurses, sterile processing, housekeeping, and even patients’ family, to know much more reliably when to expect the patient to enter and leave the operating room. For hospitals, not only does adopting Leap Rail result in higher utilization and efficiency across the OR, it contributes to patient, surgeon and staff satisfaction.”
Lack of training and communication among staff may cause a breakdown in turnover, Homan expressed. “Inefficiencies in the OR can be attributed to a lack of communication between department managers, clinical staff and OR turnover teams, a lack of training and standardized processes, and not having the right cleaning tools and chemistries at the point of use. Products alone don’t improve thoroughness of cleaning or significantly impact turnover time, and neither does monitoring or training. Think of this as a formula that combines product, process and practice. You need all three in order to deliver high quality, consistent performance.”
She proposed the Ecolab OR Program to improve process consistency and results. “The Ecolab OR Program delivers standard environmental hygiene to drive quality, consistency and efficiency through evidence-based practices, resulting in proven and sustainable results. In addition to chemistry, cleaning tools, training and consultative service, the digital dashboard with real-time reporting enables managers to track high-touch object cleanliness and turnover time in operating rooms so that targeted performance feedback can be shared with turnover teams. The Ecolab OR Program delivers faster OR turnover time, improved cleaning results, a reduced risk of HAIs, enhanced operational efficiency, process standardization and consistency, and ensured compliance with professional guidelines from organizations such as AORN and AHE, all of which contribute to measurable improvements in clinical, operational and financial metrics for the hospital.”
The program has generated better cleanliness, staff satisfaction, cost savings and turnover times, she reported. “A 576-bed quaternary care hospital with 27 ORs performing 23,000 surgeries a year implemented the OR Program. Within two months of implementation, they improved between-case high-touch object cleaning by 66%, decreased room turnover time by an average of 21 minutes and increased staff retention to 86-100%. These efficiencies helped the hospital achieve a significant cost savings with each room turnover.” 1
Change of staff can interfere with the turnover process and costs, says Champion of Cardinal Health. “Speed and efficiency are important, yet difficult to achieve. OR time is money. The biggest breakdown in an OR’s revenue generation is during room turnover and room setup; from patient out to patient in. Another huge challenge is that in every facility, the people turning over the room may be different. Environmental services departments and janitorial staffs can have high turnover rates, making it very difficult to maintain consistency. Balancing these can be quite the tap dance at times.”
Moving patients, procedure types and inconsistent cleaning processes may interrupt workflow, she added. “Transitioning patients from the OR to the PACU—if the patient is difficult to move safely for any reason, can slow down turnover. What shape was the room in last? Was the previous case a trauma or a carpal tunnel surgery? Some surgeries are definitely messier than others. Also, what procedure are you preparing for next? Based on the complexity of the next procedure, turnover could stall, as some procedures take longer to prepare for than others. A consistent process is the most important factor for successful turnover. One of the most important contributors to consistency is having the right supplies to effectively clean up; then having the right supplies to successfully prepare the room for the next procedure.”
She advises Cardinal Health’s Presource OR Turnover Kits and Presource Kitting Solutions for OR Setup to keep the OR clean and moving. “The products provide consistent supplies that support the particular processes of any facility. They promote efficiency and inspire confidence for the end user that the correct products to turn the room are available, and reliable.”
The products have shortened setup timing, she affirmed. “We are an integral part of maintaining turnover and setup efficiency, allowing the OR to stay on schedule. Time is very important to patients and caregivers as well, and an efficient OR means that procedures start on time! In speaking with our customers, we often hear, “We don’t know what we’d do without Presource kits!” Having the confidence to do their jobs effectively means everything to the end user. When we can turn over the room effectively and let the clinicians move on to the next surgery, everyone’s just happier.”
References
1. Kramer M and Kriznik S. The impact of an OR environmental hygiene program on OR culture and cleanliness. OR Manager Conference; Las Vegas, NV; Oct. 21-23, 2016.
About the Author

Ebony Smith
Ebony Smith was previously Managing Editor for Healthcare Purchasing News.