If you’re being scoped, shouldn’t that scope be tested first?
A little more than six years ago, I graduated from the Baker College Certified Surgical Technology program in Clinton Township, Michigan. I completed my clinical rotation in a large hospital and hoped to get hired there. Instead, I was hired within a couple of weeks of graduation by a small, rural facility in Michigan.
In a relatively short time, I was thrilled that my earlier hopes of working in a large facility didn’t come true. For approximately 22 years of my adult working life my previous background was in automotive-related manufacturing. As a general laborer, supervisor and eventually plant manager, I worked within various quality systems and quality standards, and intended to bring that experience to my new career. The small facility where I now was employed requires a surgical technologist background to work in the Central Service Department. Responsibilities include performing decontamination, inspection, packaging, sterilization and transport procedures, to name a few. I am still excited to be involved in the entire surgical process from beginning to end.
Because I had limited training in the Central Service Department, I relied on the guidance of my fellow Surgical Services Department staff, written policies and procedures, as well as the seemingly endless manufacturer’s instructions for use (IFU). As far as reprocessing flexible endoscopes, we had the most current reprocessing guide and up-to-date policy/procedures, which we followed religiously.
In manufacturing, a motto that I lived by was “inspect what you expect.” I carried this over into my new career to provide the best patient care possible. We understood that following the endoscope reprocessing instructions would result in the scope being adequately clean and ready for high-level disinfection (HLD) in our automated endoscope reprocessor (AER). In 2015, our facility received a package containing sample products for testing flexible endoscopes, along with documents referencing standards and guidelines from associations such as AAMI, SGNA and AORN. Prior to this our facility had no means of conducting verification testing. This opportunity was brought to our Infection Prevention Committee (IPC) which supported performing the testing if it was available. We purchased the EndoCheck-P product.
The EndoCheck-P is a swab test that detects residual protein in the biopsy channel after manual cleaning. The swabs come in a variety of sizes, corresponding to the channel diameter. According to the label and validation testing provided, the test can detect down to 1.0 µg of protein. Testing was performed on a small sample size for a year and half totaling 46 EndoCheck tests, resulting in zero failures.
McKenzie Health System (MHS) is very interested in quality and patient safety. Results were again presented to the IPC as well as an opportunity with EndoCheck to test 100 percent of scopes. IPC supported the study, which began on Sept. 17, 2017. For consistency, one employee performed all of the manual cleaning and test verifications. The manufacturer of the cleaning verification test was not present at any point and had no involvement during cleaning, testing or test result interpretation.
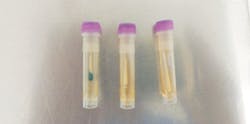
With EndoCheck-P testing, manual cleaning is completed, a swab is inserted into the instrument channel through the biopsy port and is fed all the way through, and then out of the distal end of the insertion tube, as shown in Figure 1. The swab is then cut off into a vial of reagent. At the 5-minute mark, if there is any blue/green discoloration in the fluid or on the swab, it is considered to have failed the test. Figure 2 shows a gastroscope failure for the first test of the study, from the first patient of the day.
All photos courtesy of McKenzie Health System and product courtesy of
Healthmark Industries.
The blue/green discoloration indicates residual protein that remained in the channel after manual cleaning. The discoloration in this photo is present all the way around the swab.
Cleaning progression with smudge failure
The next failure was from a colonoscope and had worse results than the first failure. Consequently, the scope had to be reprocessed two more times before it passed. I wondered what was different about the scopes that had passed versus the scopes that failed.
In this initial study, a total of 204 tests for residual protein were performed. Approximately two-thirds of the tests were conducted on colonoscopes and one-third on gastroscopes. We found four different failure types that we defined and categorized accordingly:
Figure 1 – Smudge, prior to reagent. Discoloration on the swab as it exits the insertion tube, prior to being placed in the reagent. We observed red and yellow-brown discoloration. The discoloration appears to be “smeared” on the swab as opposed to broken-up or in pieces.
Figures 2 & 5 – Smudge, post reagent – upon exiting the insertion tube, there is no visible discoloration on the swab. Discoloration is only visible after the swab was placed into the reagent.
Figure 3 – Cluster. Observed close-up, there appears to be round, grape-like clusters only visible after the swab was placed into the reagent. This example helps to differentiate the smudge type failure.
Figure 4 – Flakes. This type of failure had an interesting origin. Black and brown particles with sharp, defined edges were present as the swab came out of the distal end of the insertion tube, prior to reagent. After much investigation, we found that the flakes were intermittently injected into the scopes after manual air purging of the rinse water during manual cleaning. The inside of the air fittings were corroding, and flakes were being blown into the scopes. While trying to find the cause, we tested many scopes after HLD in the AER and there were no failures. The AER was removing any flakes that may have been present.
Figure 5 shows the first test failure on the left. The middle vial represents the second test failure after the scope was completely reprocessed. The third vial on the right shows a passing result after the scope was once again completely reprocessed. The discoloration appears to be “smeared” on the swab as opposed to broken up or in pieces.
General Information
All of the above information, as well as the information preceeding, is from Test Phase 1, consisting of 204 endoscopes with EndoCheck-P .
Colonoscopes tested: 133
- Percent colonoscope failures, not including flakes: 10 percent
Gastroscopes tested: 71
- Percent gastroscope failures: 8 percent
We are conducting Testing Phase 2 with approximately 200 additional endoscopes. We have incorporated two minor protocol changes. We changed enzymatic cleaner (selecting a cleaner with more surfactants), and two employees will perform manual cleaning and the verification testing. Test results will again be recorded along with the employee performing the testing. Testing Phase 3 will follow with another 200 endoscopes. Data from these studies will be compiled into follow-up studies, which will be published.
The question remains, should a flexible endoscope that is to be used for a procedure, be tested? For facilities without an AER, and do not test, there is a risk that what you see on those swabs could be present inside the channnel and remains there during HLD. There is opportunity for microbes to be mixed in with the protein, or other potential substances could be lodged inside the biopsy channel.
MHS’ protocol is 500ml of fluid is suctioned through the channel at bedside cleaning. During manual cleaning, we brush the channel with two passes and then suction another 500 ml of clean water/enzymatic solution through the channel. We add via syringe 90 ml of clean water/enzymatic solution into the channel to remove air where it remains for 3 minutes. Finally, we flush 90 ml of reverse osmosis water through the channel to remove remaining detergent/debris. We were following the instructions supplied by the device maufacturer. In many cases, we had to complete the above procedures on some scopes several times to obtain a passing test result. Results support the importance of utilizing a verfication testing process, such as EndoCheck P.
When it comes to the highest quality of patient care, I remember my favorite quote from W. Edwards Demming: “It is not enough to do your best; you must know what to do, and then do your best.” This verification process ensures we are providing the best patient care for those who choose to get scoped at our facility.
Spencer gives special thanks to Healthmark Industries for supplying the EndoCheck-P protein cleaning verification products used in this study, but notes that the company played no part in interpretation of data or results. Spencer also thanks his colleagues and coworkers for supporting the study.
SCOPES:
Single-use endoscopes: Pop fly or home run in cleaning, sterilization?
Reusable endoscopes: Tried and true for cleaning
Tips, tools and tricks for inspecting properly cleaned endoscopes