There are so many different kinds of wounds: surgical incisions and other cuts, burns, diabetic ulcers, pressure sores, ostomies, and more. Some wounds are acute and some are chronic. Their needs for optimal healing are different, but they all must be protected from potential infection.
Protecting the skin
The skin is our first-line of defense against infection, so it is important to keep it healthy and intact. Skin rendered raw by incontinence is more susceptible to infection, and damaged skin can be very painful for the patient. Traditionally, a moisture-barrier paste has been used to protect damaged skin, but paste can have drawbacks. Debra Thayer, MS, RN, CWOCN, Lead Technical Service Specialist, 3M Health Care, Critical and Chronic Care Solutions Division, explained how 3M has improved on barrier treatments, in response to clinicians’ request for a more effective approach to severe cases of incontinence-associated dermatitis (IAD).
“Incontinence-associated dermatitis is increasingly recognized as a problematic and preventable form of skin injury,” stated Thayer. “Exposure to stool and/or urine is the primary causative factor, creating top-down injury through inflammation, often in combination with friction.
“A common approach to protect denuded skin involves application of a moisture-barrier paste,” Thayer continued. “Although readily available and relatively easy to apply, pastes can have significant limitations for both patients and clinician. The extensive experience of 3M in coatings and medical polymers led to the development of an innovative barrier technology. 3M Cavilon Advanced Skin Protectant is a high-endurance skin protectant designed to stop, reverse, and prevent the damaging effects of moderate to severe IAD. It is designed to provide skin protection under the most challenging conditions of irritant exposure.”
Unlike paste, 3M Cavilon Advanced Skin Protectant is long-lasting, so the patient’s raw skin does not have to be subjected to frequent treatment. Another advantage is its elasticity. Thayer expounded: “The polymer-based barrier creates a highly protective coating on the skin, with exceptional durability that allows the barrier film to elongate and stretch during wear. This elastomeric property ensures integrity even when exposed to caustic, corrosive irritants such as liquid stool and gastric fluid. Durability also allows for extended wear, with only two to three applications needed. The skin protectant creates an effective, long-lasting barrier on both intact and wet, weeping skin. The unique barrier is breathable and comfortable through application, wear, and the cleansing processes, protecting for up to seven days and wearing away naturally.”
Cavilon Advanced Skin Protectant saves clinicians time with its easy-to-use, single-use applicator, which speeds up the application process and decreases the potential for contamination associated with multi-use tubes. “The skin protectant can also help reduce the risks that contribute to pressure injuries,” added Thayer. “A once painful experience for patients, and a time-consuming process for clinicians, Cavilon Advanced Skin Protectant helps ease the burden of both having and managing IAD.”
Pressure ulcers are another painful skin condition at risk for infection. Pressure ulcers often start on the operating table, particularly when procedures last more than two hours or when the patient is older and has thinner skin, or perhaps is emaciated, placing more pressure on bony prominences, or has underlying conditions such as diabetes.
Clearly, prevention of pressure ulcers is always the best-case scenario. Randy Schwartz, Vice President of Marketing, Mölnlycke Health Care, told Healthcare Purchasing News about Mölnlycke’s recently released products designed with prevention in mind. “As the science behind wound management evolves, it opens up new opportunities to improve wound-care products and solutions. Mölnlycke combined many types of research — clinical, scientific, and health economic research — when developing and updating our Mepilex Border Sacrum and Heel, along with the introduction of our new Mepilex Border Post-Op Ag. Mepilex Border Post-Op Ag was designed to meet the specific challenges of the postoperative patient, whereas the updated Mepilex Border Sacrum and Mepilex Border Heel targets pressure-ulcer prevention.”
Mepilex Border Post-Op Ag is an antimicrobial dressing that provides rapid, sustained release of ionic silver. It also includes Safetac, a Mölnlycke proprietary technology that minimizes dressing-related pain to the patient and trauma to the wound.1 Schwartz explained how it works: “Mepilex Border Post-Op Ag antimicrobial dressing supports early patient mobilization through unique, flexible cuts in the absorbent pad specifically designed to remain in place and absorb excessive blood or exudate, keeping patient comfort and quality-of-life issues in mind.”
Other attributes of Mepilex Border dressings include improved user features for easier handling. “Mepilex Border Sacrum has been enhanced with product handling tabs, to enable skin checks, plus additional protection and sealing tabs at the gluteal cleft. The upgraded Mepilex Border Heel dressing has an increased foam-surface area and expanded ankle coverage,” said Schwartz.
“Surgical-site infections (SSIs) and pressure ulcers represent two of the most costly and potentially dangerous wound-management challenges,” continued Schwartz. “With pressure ulcers, not only does prevention help patients avoid a painful and debilitating injury, it ultimately saves hospitals money. A 2017 study of more than 1 million patients showed that prophylactic use of Mepilex Border dressings offered a return on investment of 100 percent within just one year and could save hospitals $200,000 to $600,000 per year on PSI-03 [AHRS Patient Safety Indicator #3 ] expenses.2 In a study of 262 coronary artery bypass graft patients in a 32-month period, Mepilex Border Ag was a valuable part of a bundled SSI-prevention approach. A 3.74 incidence per 100 procedures was reduced to 0.7, and ultimately to 0, with a cost avoidance of $606,498, with 377 excess hospital days avoided.”3
Schwartz said it can be tempting for purchasers to choose the least expensive product when they look similar and reference the same clinical literature. “But looks can be deceiving,” he said. “While you might save $1 per dressing in upfront costs, an SSI or pressure ulcer can quickly negate initial savings, and that’s before a potential lawsuit. We firmly believe that clinicians and purchasing professionals must factor in the evidence when making buying decisions.”
Fishing for options
When a wound doesn’t heal, a skin graft may become necessary. A new and interesting option in skin-graft technology is available from Kerecis. Their product is derived from fish skin. Fish skin may not be your first thought for optimal skin grafting, but apparently it reaps good results. Gunnar Johannsson, MD, Head of Medical Affairs, Kerecis, explained how they arrived at this solution and its advantages to recipients. “We see an increasing focus on natural rather than synthetic solutions. One new development is the use of fish-skin—based skin substitutes. Fish skin is much more similar to human skin than other skin substitutes and has the healing benefits of Omega-3, which relieves pain, reduces inflammation, and provides a barrier for bacterial growth. Because no disease transmission risk exists between codfish and people, the Omega-3—rich Kerecis product is only minimally processed, preserving all of the skin’s natural components.” Johannsson said that, when grafted onto damaged human tissue, “the acellular material recruits the body’s cells from the wound perimeter. These cells are incorporated into the fish skin, which is ultimately converted into functional, living tissue. The material has been shown to accelerate healing and regenerate damaged human tissue.”
Johannsson said that use of Kerecis Omega-3 fish-skin graft-transplantation technology also has the potential to reduce healthcare costs.4 “Treating wounds well at the onset makes good economic and medical sense. Left untreated, a serious wound can lead to amputation, which is expensive in terms of services and in human cost. Even if a chronic or hard-to-heal wound is not that serious, it requires ongoing medical attention, which can increase the cost of treatment and diminish the quality of life.” Johannsson cited a study comparing the cost of using Kerecis’s solution with a more traditional product. “A podiatrist at the American Health Network in Indianapolis compared the cost of treating 27 diabetic foot ulcers with the Kerecis product with the cost of the standard-of-care treatment. The study concluded that the fish-skin treatment saved an estimated $65,000.”5
Johannsson provided a glimpse into the future of skin-graft technology. “Instead of focusing on a single protein, growth factor, or matrix, we expect to see more intact products with all the elements needed to activate the body’s cells for healthy tissue regeneration. Especially interesting are the studies being done on lipids in the wound environment.”
Preventing surgical-site infection
In their updated “Guideline for the Prevention of Surgical Site Infection, 2017,”6 the Centers for Disease Control and Prevention (CDC) estimated that, in 2006, approximately 80 million surgical procedures were performed in the United States, and that between 2006 and 2009, SSIs complicated approximately less than two percent of surgical procedures in the United States. The CDC also indicated the number of SSIs is probably underestimated, since approximately 50 percent of SSIs become evident after discharge. The CDC estimated mean attributable costs of SSIs range from $10,443 in 2005 to $25,546 in 2002 per infection. Costs can soar to $90,000 per infection when the SSI involves a prosthetic joint implant or an antimicrobial-resistant organism.” Despite these astounding numbers of infections and related costs, the CDC states, “Surgical site infections are persistent and preventable healthcare-associated infections.”
Clearly, attention to infection prevention should be observed in the surgical suite, starting with clean healthcare-worker hands. Joey Suntken, Vice President of Marketing, Healthcare, GOJO, talked about the attributes of their waterless surgical scrub. “PURELL Waterless Surgical Scrub provides germ kill and persistent activity critical to the surgical environment. PURELL Waterless Surgical Scrub’s alcohol formulation is designed to meet and exceed U.S. Food and Drug Administration (FDA) requirements for surgical scrubs without ingredients that cause skin damage.
“In 2017, the Association of Perioperative Registered Nurses (AORN) updated its hand-hygiene guidelines,” stated Suntken. “Previously, AORN guidelines recommended that ‘an alcohol and chlorhexidine product that is fast drying and has residual effect is preferred.’ Based on AORN’s comprehensive review of the literature, the new guidelines no longer state that a product containing chlorhexidine gluconate is preferred. Instead, AORN recommends a healthcare facility’s team should select products for hand hygiene and surgical hand antiseptics that meet FDA requirements,” said Suntken. “This means product selection should be driven by overall performance of the product against FDA efficacy requirements and not specific active ingredients.”
Suntken said that PURELL Waterless Surgical Scrub requires only two applications and dries quickly. “It creates a pH-balanced environment that helps inhibit germ recovery and regrowth, and, as a result, is able to provide six-hour persistence without the need for a secondary active. PURELL Waterless Surgical Scrub can be used in operating rooms or other high-risk areas.”
Liza G. Ovington, PhD, FACCWS, FAPWCA, MWC, Medical Director, CER, Wound Healing & Infection Prevention, Ethicon, part of the Johnson & Johnson family of companies, explained that, whereas medical devices such as knee implants or pacemakers are clearly foreign bodies with the potential to create risk for surgical infection, it might not be so obvious that sutures, including absorbable sutures, are also foreign bodies.
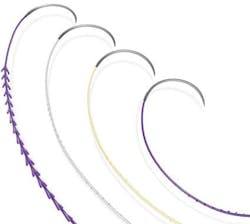
Because bacteria can colonize the suture surface and develop a biofilm resistant to phagocytic immune cells and antibiotics, there is the risk for developing an SSI. “Any suture product of natural or synthetic composition and of mono- or multi-filament construction is susceptible to bacterial attachment and colonization,” explained Ovington. “This risk factor can be addressed by coating the suture surface with an antibacterial agent that kills bacteria and prevents biofilm formation. Ethicon’s triclosan-coated sutures represent a targeted intervention to address the specific risk factor for SSI posed by the presence of suture as a foreign body in the wound. Ethicon’s Plus Sutures (VICRYL Plus Antibacterial Suture, MONOCRYL Plus Antibacterial Sutures, PDS Plus Antibacterial Suture,) have been clinically evaluated in multiple independent clinical studies involving over 19,000 patients and a wide variety of surgical-procedure types. These clinical studies have been performed in over 23 countries and have been published in the peer-reviewed medical literature.”
Ovington cited the 2017 meta-analysis of Plus suture data by Wu et al, which examined 18 studies.7 “Their meta-analysis demonstrated that antimicrobial sutures reduced SSI risk by 28 percent for the randomized studies and by 41% in the cohort studies.” These authors also concluded that the effect of antimicrobial coating was similar between different suture, wound, and procedure types.
The most recent meta-analysis, by Leaper et al, examined 34 clinical studies on Plus sutures from 2005 through 2016.8 “Their analysis demonstrated that, compared to non-antibacterial sutures, the use of Plus sutures was associated with a 39 percent reduction in the risk for SSI.”
The World Health Organization’s recommendation on use of antimicrobial sutures in their 2016 ‘Global Guidelines on the Prevention of Surgical Site Infections’ was based on Wu et al’s findings,”7 Ovington said. “Their recommendation states, ‘The panel suggests the use of triclosan-coated sutures for the purpose of reducing the risk of SSI, independent of the type of surgery.’” Ovington added, “Recommendations for use of triclosan-coated sutures have also been included in the American College of Surgeons and Surgical Infection Society ‘Surgical-Site Infection Guidelines 2016 Update,’ and the CDC ‘Guideline for Prevention of Surgical Site Infection, 2017.’”6
References
1. White R. A multinational survey of the assessment of pain when removing dressings. Wounds UK 2008;4(No 1):14-22. http://www.wounds-uk.com/pdf/content_9188.pdf. Last accessed June 28, 2017.
2. Padula WV. The real-world effectiveness and value of sacral dressings to prevent hospital-acquired pressure injuries in academic medical centers: an observational cohort study. Presented at the Symposium on Advanced Wound Care; San Diego, CA; April 2017. Poster.
3. Kles CL, Murrah CP, Smith K, et al. Achieving and sustaining zero: prevention of surgical site infections after isolated coronary artery bypass with saphenous vein harvest site through implementation of a staff-driven quality improvement process. Dimens Crit Care Nurs. 2015;34(5):265-272.
4. Magnusson S, Winters CL, Baldursson BT, et al. Acceleration of wound healing through utilization of fish skin containing Omega3 fatty acids. Today’s Wound Clinic. 2016;10(5). http://www.todayswoundclinic.com/articles/acceleration-wound-healing-through-utilization-fish-skin-containing-omega-3-fatty-acids.
5. Magnusson S, Winters C, Hermannsson GM, et al. Cost saving potential of acellular fish skin graft: a cost simulation study on diabetic foot ulcers. Presented at the Symposium on Advanced Wound Care; Las Vegas, NV; October 2016.
6. Berríos-Torres SI, Umscheid CA, Bratzler DW, et al. Centers for Disease Control and Prevention guideline for the prevention of surgical site infection, 2017. JAMA Surg. Published online May 03, 2017. http://jamanetwork.com/journals/jamasurgery/fullarticle/2623725.
7. Wu X, Kubilay NZ, Ren J, et al. Antimicrobial-coated sutures to decrease surgical site infections: a systematic review and meta-analysis. Eur J Clin Microbiol Infect Dis. 2017;36(1):19-32.
8. Leaper DJ, Edmiston CE Jr, Holy CE. Meta-analysis of the potential economic impact following introduction of absorbable antimicrobial sutures. Br J Surg. 2017;104(2):e134-e144.
About the Author

Susan Cantrell
Susan Cantrell is Infection Prevention Editor for Healthcare Purchasing News.