Hospitals sustained huge financial losses during COVID-19
A new report details how the impact that postponement of nonessential surgical procedures early in the coronavirus pandemic disrupted surgical care at U.S. hospitals, and also took away a large portion of hospitals’ total income, results from two studies reveal. These findings (from the two studies, which took place at the University of Pennsylvania, Philadelphia, and Children’s Hospital of Philadelphia) were presented at the virtual American College of Surgeons (ACS) Clinical Congress 2021 and reported in a release.
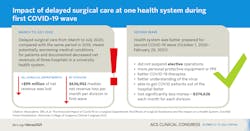
Surgical services are typically an important financial engine for hospitals, and the new study findings showed that curtailing surgical procedures for even two months can seriously impact a hospital’s financial security. Most elective, nonurgent operations in the country stopped from mid-March to early May 2020, to conserve resources for patients with coronavirus disease 2019 (COVID-19). Results of one study found that this two-month suspension cost a single university healthcare system 42 percent of its net revenue for five months.
Nationwide, hospitals lost $1.53 billion from missed elective pediatric procedures alone, the other study investigators estimated as part of their study, for approximately the same period, March to May 2020. Hospitals were slow to make up the surgical backlog and the lost income from children’s operations, with a median, or middle, time to recovery of one year, the investigators estimated.
As COVID-19 cases reportedly continue to remain high in many states, some hospitals are again triaging cases and delaying selected operations. Consequently, the researchers said, their findings demonstrate the need for better long-term planning by hospitals to prevent further shutdowns to ensure patients have access to the surgical services that they need.
The pandemic resulted in an unprecedented temporary postponement of many elective operations across the country, as recommended by the American College of Surgeons (ACS) and other organizations in March 2020 to free hospital beds and other resources for COVID-19 patients. The ACS provided guidance for how hospitals could triage surgical cases—that is, select which operations to prioritize and which to defer until after COVID-19 caseloads decreased.
Dr. Mazzaferro and his coworkers calculated the net revenues of three hospitals in their healthcare system during the first surge, or “wave,” of COVID-19 cases from March to July 2020, compared with the same period in 2019. A total of more than $99 million of net revenue was lost from all surgical departments and $58 million from the department of surgery in the first wave. The researchers reported a median net revenue loss of $636,952 per month per division for the department of surgery in the first wave, using updated data presented during the virtual Clinical Congress. However, the system lost significantly less money—$274,626 each month for each division—during a second COVID wave between October 1, 2020, and February 29, 2021.
The surgical department did not suspend elective operations during the second surge, said Liza Wu, MD, FACS, senior investigator of this study and professor of surgery at the Perelman School of Medicine.
“We were in a better position than the first time around to continue with elective surgery,” Dr. Wu said. “We had more personal protective equipment or PPE, better COVID-19 therapies, and a better understanding of the virus, and we probably were able to get COVID patients out of the hospital faster.”
Their surgical department, she added, also began triaging elective surgical patients using a new scoring system called the Medically Necessary, Time-sensitive Scoring, or MeNTS, which University of Chicago physicians described in the Journal of the American College of Surgeons.
After elective operations resumed in June 2020, surgeons quickly regained their productivity, Dr. Mazzaferro reported. He made this conclusion based on a measure of surgeon productivity that insurance payers use for reimbursement, called work relative value units (RVUs). Work RVUs decreased significantly less in the second COVID-19 wave than the first: 7.8 versus 13.2 percent.
For the second study, researchers led by Sourav Bose, MD, MBA, MSc, then a postdoctoral research fellow at Children’s Hospital of Philadelphia, assessed the financial impact of COVID-related pediatric procedural cancellations. To project lost surgical revenues, they used the 2016 Kids’ Inpatient Database, which represents approximately 80 percent of pediatric hospital admissions nationally.
Dr. Bose, a General Surgery Resident at Brigham and Women’s Hospital in Boston, said the nation’s children’s hospitals delayed or canceled an estimated more than 51,000 elective procedures from March to May 2020.
Dr. Mazzaferro also recommended that healthcare systems make long-term preparations so they can safely provide elective surgical care during future peaks in COVID-19 caseloads. He suggested the following:
- Increase hospital bed and resource capacity through alternate solutions, such as sending an overflow of surgical patients to other patient care units or facilities that can accommodate them.
- Appropriately triage elective operations following ACS guidelines4 and other published surgical triage tools.
- Ensure sufficient PPE for health care workers and patients.
- Help keep staff healthy by mandating COVID-19 vaccines or frequently testing them against the virus.