In the game of baseball, you might be surprised to learn that singles and bunts win more games than home runs. While a home run can sometimes win a game, it is important not to overlook the smaller, yet significant steps within budget management, particularly in today’s healthcare environment where reimbursement is diminishing and costs are escalating. Yet those who manage budgets often strive for home runs in savings. The truth is, almost twice as many games are won with singles, not home runs.1 If we can rely on this small gain strategy, we are more likely to be able to reduce our expenses.
Altru Hospital is a community healthcare system with 15 operating rooms in its main hospital, which is located in Grand Forks, ND. The Altru Specialty Center, where the weekly cataract surgeries take place, is located a few miles away from the main hospital and contains four operating rooms and its own Central Sterile (CS) department.
Altru Hospital and SolutionWells teamed up to strategically target eye instruments that frequently get damaged and test the hypothesis that using custom trays will reduce repair expenses. Altru also began looking at custom trays as a way to protect their eye instruments as they prepared to build an off-site eye center that does not have its own CS department. Transporting the eye instruments from the main hospital’s sterilization facility to the new eye surgery center created the possibility of more damage to their fleet of instruments.
With the goal of saving money on maintenance costs, let’s look at some ideas for hitting more singles in order to try and win the repair-budget game.
Study overview
For this preliminary report, three years of historical instrument repair data was collected to establish a benchmark, which we used to compare to three months of repair data collected after custom trays were introduced to hold existing instruments. For the most accurate outcome, we will continue tracking the data in this study for another nine months so that we have one full year of data using custom trays.
The first study, which will wrap up in late 2017, focuses on the first quarter of a year-long analysis to evaluate the impact that custom trays have on repair for surgical eye instruments and staff efficiency. These year-long findings will be published in 2018.
The second study, to be shared later this year, will evaluate trays designed to eliminate hand-washing of rigid telescopes in favor of following the instructions for use (IFU) for machine washing these expensive and valuable instruments used during minimally invasive surgery (MIS).
The third study looks at compliance, accountability, and how that may affect outcomes for study number two. These findings will be reported in another article in 2018.
This work aims to provide valid information that hospitals could use to develop a strategic plan that would reduce spending by hitting a “single” in a specific specialty. Three questions this study will clarify are:
- Does it make sense to spend money on custom trays?
- Do custom trays reduce damage for expensive instruments?
- Do custom trays have any impact on staff efficiency?
Analyzing the resulting information will provide insight that will help determine if the hypothesis — switching to custom trays lowers repair costs — could become theory.
Specifics
When we designed this analysis, we knew that it would have some problematic variables. For instance, the instruments used in the cataract trays were well-worn prior to the study and we expected breakage during the trial. Regardless of the possibility of damage to older equipment skewing the results, we felt this study important enough to implement. The goal of the study was to test the custom trays while the OR and CS staff continued functioning as usual (i.e., using custom trays was the only change). This study is a real day-to-day look at how moving legacy instruments into custom trays may or may not affect repair strategy.
It’s also important to note that in August 2016 nine new additional sets of instruments went into circulation because there were not enough sets previously to supply surgeons for a full day of cataract cases. To start the study and prepare for a move in 2017 to Altru’s new facility, new custom trays were introduced December 2, 2016. Since these variables complicated using 2016 as a repair benchmark, it made sense to average data over three years to minimize variables introduced from one year.
When one looks at the cost of a specific fleet of instruments (e.g., Cataract Tray, Neuro Tray, CV Tray, Digital Ureterscope Tray, etc.) it makes sense to protect that investment and try to lengthen its longevity. This may seem difficult, especially when so many people are handling the trays every day, which is why we must first consider the value of what we are using and understand the true cost of keeping it running with precision. These two factors are extremely important when caring for patients and keeping them safe.
Another formula we used to predict and track repair is instrument failure rate (IFR). For example, Altru Hospital’s fleet of cataract instruments are worth $137,292 and the most they spent on annual repair and replacement expenses was $12,189 in 2015. But on average, Altru was spending $7,361.12 annually to repair their cataract instruments. The IFR is an easy way to benchmark and explore improvement or a loss for a specific fleet of instruments and provides an additional way to assess, predict and justify how specialty instruments are performing.
Once we established and understood these key points, we made sure that everyone who comes in contact with this equipment was educated and willing to be accountable for its handling — although the goal also was to stop assigning blame for instrument breakage and instead identify the cause and find solutions for avoiding future damage.
Examining the data
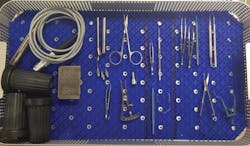
The trays used prior to this study had silicone finger-mats in the bottom of the trays with hooks and Sweeney manipulators that may have been contributing to some of the damage. Also, the silicone finger-mats did not hold the instruments securely, and occasionally they would escape the tray and fall into the ultrasound cleaner during decontamination (see Figure A).
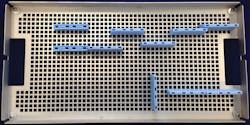
The new trays hold the instruments in place 360 degrees and eliminated the need for finger-mats because the silicone holders in the lid mated perfectly with the silicone holders in the bottom of the tray (see Figures B and C). When assembled, the instruments are incapable of moving. These types of trays typically sell for $1,400 to $1,500 per tray.
Between 2014 and 2016, Altru has been spending an average $613 per month for repair of their cataract instruments. During the three-month period, the average monthly expense to repair and/or replace inventory dropped to $417. Altru’s instrument failure rate (IFR) also fell from 18 percent to 3 percent. When comparing to early results in 2017, this change is significant. The remaining nine months of this study will give valuable information to further support or reject the hypothesis that custom trays decrease repair costs.
The first phase of this study shows that using custom trays should reduce repair expenses for Altru Hospital. Averaging the data from 2014 to 2016 blends in the variables that took place in 2016 and gives a more accurate picture of what can happen when one focuses on hitting singles.
If 2017 reflects what the extrapolated numbers suggest, Altru can expect to save 32 percent per year by using custom trays to protect their eye instruments (see Figure D, below).
(three years)
Figure D
Efficiency, time savings
The study also seeks to find out if the use of custom trays would have an impact on staff efficiency. Each tray has three zones:
- Zone A is for keeping instruments used by both of the surgeons.
- Zone B is for instruments used exclusively by surgeon B.
- Zone C is for instruments used exclusively by surgeon C.
The old tray used two finger-mats; one was placed underneath the instruments and the second finger mat was placed on top of the instruments to attempt to hold them in place. Prior to the start of the study we timed how long it took one of the CS techs to assemble all the clean instruments in the appropriate zones after they came out of the washer. Using the old tray, it took 8 minutes to assemble compared to 7 minutes it took using the new custom tray. The finger mats retain a significant amount of water after coming out of the washer and must be shaken until reasonably dry. This extra task accounted for the time difference in assembling the trays. (A study by Ofstead, etal shows that a CS Tech costs a hospital $16.80 per hour or $0.28 per minute on average.2 During our study of 119 cases, the one-minute difference assembling the trays would save the hospital $33.32 per quarter or $133.28 per year.)
Conclusion
This preliminary study suggests that implementing custom trays with a designated home that secures each instrument from above and below yields a significant repair expense savings of 32 percent a month. IFR also enabled us to see if repair expenses were reduced during specific timeframes. For instance, in 2015, the eye trays were experiencing an IFR of 18 percent of the value of their fleet (damage per year equals $12,189 divided by $68,643, the value of their entire inventory of eye instruments sets). Within three months we saw that figure drop to 3 percent. We will revisit this data at the end of 2017 to see if repair expenses increase or continue falling.
References
1. Granillo, L. (2009) http://baseballanalysts.com/archives/2009/08/walking_off.php.
2. Olfstead, C.L., Quick, M. R., Eiland, J.E., and Adams, S.J., (2017).