CS Connection
With growing procedural volumes, the increasing complexity of medical/surgical instruments, and a healthcare industry under mounting pressure to improve patient care and safety, the central sterile/sterile processing department (CS/SPD) is one of the busiest and most stressful places to work. CS/SPD professionals are expected to effectively reprocess instruments and get them back into the hands of clinicians as quickly as possible. The challenge lies in balancing the demands for quality work with the demands for speed.
In this article, we present advice and best practices from CS/SPD professionals and other industry experts on how to improve reprocessing workflow efficiency throughout the process without compromising patient safety.
Best practices at each reprocessing stage
As with any process, efficient and effective reprocessing of surgical instruments requires staff members at each stage to perform their tasks correctly the first time, eliminating the need for time-consuming rework.
Point of use
When operating room (OR) staff members fail to clean instruments after use, it can lead to a snowball effect of reprocessing delays. In cases where blood, tissue and other organic matter dries and hardens on instruments from the time they are used to the time they reach decontamination, the CS/SPD team’s job becomes even harder as they attempt to remove this bioburden.
Arlene Bush CRCST, CER, CIS, CHL, SPD Educator at AdventHealth Orlando and Communications Director for the IAHCSMM Central Florida Association of Central Service Personnel (CFACSP) Chapter, explains how education of OR staff on the importance of point of use cleaning has played a huge role in improving her department’s reprocessing workflow efficiency.
According to Bush, education started at the top with required in-services for department heads, supervisors and frontline staff to set expectations for required point-of-use cleaning. Bush and her team also opened a quality feedback option in their instrument tracking system to allow decontamination staff to enter feedback when point of use cleaning did not take place on items entering decontamination. Next they tracked compliance and reported it out in department huddles.
“Once staff understood the ‘WHY’ behind point of use cleaning, instrument thru put times increased dramatically,” said Bush. “It was a move in the right direction for reprocessing workflow efficiency and staff satisfaction.”
“Imagine this: It’s your turn in decontamination on second shift and you walk into a clean decontamination room at 3 p.m., your first case is coming down from the operating room and you’re ready,” said Castillo-Gutierrez. “It’s a coronary artery bypass graft (CABG), you open the large case cart and all the instruments are thrown into the containers, and some baskets don’t even have instruments in them. This is going to take awhile to sort, not to mention sharp hazards and trash can be seen throughout.”
After shadowing a few cases, Castillo-Gutierrez and a team of nurses, OR techs and sterile processing technicians found one process, restringing instruments after cases, offered benefits to all parties involved. It helped the OR with last counts and made it easier for staff members to place items back into correct sets. For the CS/SPD, restringing reduced decontamination time by 30 percent, decreased the number of lost instruments, protected instruments from damage during transport (e.g., placing heavy instruments on top of delicates or lids crushing instruments due to poor organization), and it helped boost CS/SPD staff safety by allowing them to easily see sharps that had been inadvertently placed facing up.
“It took a lot of in-servicing for everyone but restringing gave both sterile processing and the OR great turn-over results, earning us commendation from the Joint Commission survey for the concept,” said Castillo-Gutierrez.
Decontamination and cleaning
“One key area that CS/SPD professionals must address to improve workflow efficiency is the decontamination area where the set-up is important for instrument cleaning and processing to be completed correctly and according to instructions for use (IFU) specifications,” said Greene-Golden. “The workflow in the decontamination area must allow for the removal of instruments to the sink and adequate professional sinks that can be used to properly rinse, soak and clean trays of instruments according to the IFU. Sonic machines, washer decontaminators, flexible inspection scopes and cart washers all need to have room to function correctly in a manner that allows workflow to be seamless. The standard requirements and design can be found in the ANSI/AAMI ST79:2017.”
Michael DeFee, CRCST, CHL, SPD Manager, Riceland Healthcare, Beaumont, TX, has designed a decontamination space where technicians have everything they need close at hand.
“We are in a very busy day-surgery setting where instruments must be turned over quickly because we don’t have a lot of inventory,” said DeFee. “Designing our decontamination space took planning and experimenting to see how we could support a fast pace without compromising efficacy and safety. While our space is small, each person has exactly what he or she needs at arm’s length and can work with minimal distraction.”
Harris explains how effective and efficient practices in decontamination pave the way for streamlined cleaning in washers/disinfectors, stating:
“Instruments should be pre-cleaned in decontamination prior to being placed in the washer, and ringed instruments should be strung on an appropriate style stringer to keep them in an open position when they are placed in the washer. Best practice is to place those instruments with the finger rings down and the box locks up towards the spray arms of the washers. Instrument baskets should not be overloaded so that washer chemistries can make contact with all instruments.”
“When instrument washers were first introduced, they washed eight to 10 instrument trays per hour,” McCormick explains. “A single, three-well sink can output 12 to 15 instrument trays per hour. Most SPDs would have one sink for two instrument washers. Current instrument washers output 18 to 20 trays per hour on average, yet many facilities continue to plan one sink for two washers. By increasing the number of three-well sinks to one per washer, it will help balance workflow and reduce backlog.”
The washer/disinfectors themselves can make or break the effectiveness and efficiency of the entire process, according to Gene Ricupito, CRCST, CHL, CFER, PMP, Interim Director of SPD, UCSF Health.
“In my experience, one of the most critical process control points to address for efficiency is the throughput of mechanical washer/disinfectors,” said Ricupito. “Lengthy cycle times, idle time and unplanned downtime can greatly impact the workflow from decontam to assembly. Short of replacing older equipment with efficient cutting-edge technology, organizations should also periodically collaborate with their field service engineer to ensure that variable cycle parameters are optimized specific to the processes and other technology assets in use. While there is a careful balance between effective cleaning and the length of the cycle, there are variables that can be tailored to meet the needs for repeatable quality outcomes without over-processing devices in decontam.”
Inspection, assembly and packaging
While most of the “dirty work” is over once the instruments come out of the washer/disinfector and into the clean side of the CS/SPD, the process of inspecting, assembling and packaging instrument sets and trays prior to sterilization require proper planning, expert skills and the appropriate equipment to facilitate speedy turn around times.
“Once trays reach the clean side they should be tested for sharpness, cracks and any other types of damage that may be present,” said Harris. “Best practice is to inspect and assemble trays in the order in which they will be needed. Priority trays should be assembled first. Once trays are sterilized they should not be transferred to their storage area until they have reached ambient temperature to prevent condensation from forming in the tray.”
“Many techs assemble similar sets in the same group rather than assembling based on need,” said James Marchisio, MBA, Business Manager, Perioperative Services, The Ohio State University Wexner Medical Center East Hospital in Columbus, OH. “The long-standing culture, of ‘the sterilizer must be full’ creates unnecessary inefficiencies. A focus on productivity is important; however, clean, sterile and accurate sets are factors that must be a priority for every SPD to run efficiently.”
Sterilization
Whether a CS/SPD is using rigid containers, peel pouches or sterilization wrap, each comes with its own opportunities for workflow improvements.
With a background in medical device manufacturing, Charlie A. Webb CPP, Sterile Packaging Sciences, Van der Stahl Scientific, believes repeatability in pouch sealing is the greatest challenge facing CS/SPDs.
Reprocessing instruments used in orthopedic procedures takes a great deal of time and labor among CS/SPD professionals because of the number of sets used per case and the growing volumes of orthopedic cases, including total joint replacements (e.g. knee, hip).1
A retrospective study published at the 2019 Association of periOperative Registered Nurses (AORN) Global Surgical Conference & Expo demonstrated how Turbett Surgical's Instrument POD system, with its 15-tray capacity, cuts instrument processing time by 45 minutes or more for orthopedic instrument sterilization, compared with the use of rigid containers and sterilization wrap. The results show that 20 percent of the time savings was achieved prior to the autoclave, 70 percent observed in the POD rapid dry time and 10 percent in the transfer from the autoclave’s sterile racks to the case cart.2
“Ambulatory surgery centers (ASC) and hospitals struggle every day to support the rising number of surgeries with inadequate instrumentation,” according to Barbara Ann Harmer, MHA, BSN, RN, Vice President of Clinical Services at Innovative Sterilization Technologies, LLC. “The use of ONE TRAY dramatically reduces the wait time for completion of the sterilization cycle, dry and cool times. Faster turnaround of instrumentation voids the need for hospitals to invest in additional surgical instruments. The absence of idle time when using ONE TRAY can also drive better employee productivity as staff members could be deployed for activities such as preparations for surgeries, equipment maintenance or quality control.”
The performance and intended use of the ONE TRAY Sealed Sterilization Containers should utilize the device manufacturers’ sterilization exposure parameters and recommended practices/guidelines outlined by the Association for the Advancement of Medical Instrumentation (AAMI) and AORN.
Storage and transport
Following sterilization, CS/SPD professionals must transport sets either to a storage area, or to the OR for the next case. Melissa Lingle, MBA, BSN, RN, Director of Perioperative Services, The Ohio State University Wexner Medical Center East Hospital, comments on factors that influence workflow efficiency during transport.
“Transportation of instrumentation to and from sterile processing and the OR is different in each facility,” she said. “The proximity logistics of the OR to SPD can create inefficiencies that are difficult to streamline. Most facilities have SPD in the basement; for those that are fortunate enough to have SPD on the same level of the OR, count your blessings! Many perioperative departments must creatively design a workflow that effectively navigates the challenge of having an SPD three to four floors below the OR. Factors to consider when designing the workflow include elevator wait times, sterile pathway, transport labor requirements, surgical volume and clean return rate.”
“One of the things we hear a lot about in both the CS/SPD and OR areas is the number of torn sterile instrument packs,” said Gerber. “This contributes to a high level of frustration when tears are found causing instruments sets to have to be re-wrapped and sterilized again. Not only does this cost time and money, but if this happens just prior to a surgical procedure beginning it can lead to delaying or even canceling that procedure. The impact on the patient emotionally cannot be understated. If this issue can be addressed and virtually eliminated it would have a major impact on workflow efficiency.”
Best practices across the board
There are some best practices that a healthcare facility can apply throughout the entire reprocessing cycle to drive greater efficiency while maintaining patient safety.
Education
Proper education of staff — in both the OR and CS/SPD — lays the foundation for success and serves to boost process efficiency by reducing mistakes and rework.
“The biggest challenge to CS/SPD and workflow is education of staff in best practices of how to reprocess the select equipment,” said Mark A. Leath, President, CS Medical. “Equipment manufacturers have varying IFUs and being fully versed on each is at times hard. Staff turnover and rush to turn instruments lead to healthcare-associated infections (HAI). Furthermore, any reduction in manual process to the workflow would be beneficial. For example, when reviewing reprocessing of transesophageal echocardiogram ultrasound probes (TEE), if you could automate cleaning prior to high-level disinfection with a validated process you could improve the workflow and solve a noted problem- cleaning of reusable instruments.”
Communication
At every stage of reprocessing, communication is critical to success, explains Ralph J. Basile, Vice President of Healthmark Industries.
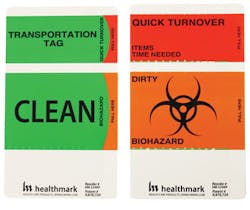
“There are many areas ripe for improvement and effective communication is key,” said Basile. “Adopting methods to alert coworkers to the condition of devices (e.g., clean, dirty, processed, etc.) is one such example. Needless to say, it is critical that only processed devices are used and a used device is fully processed. There are too many documented incidents when a device was thought to have been processed, but wasn’t, and ended up being used on a patient.”
Designed for compliance with OSHA standard CFR 1910.1030, the Healthmark Transportation Identification Tag is 3.125” x 5.125” with one perforated tab, a green top tab with “CLEAN” in black text, a fluorescent orange/red bottom tab with “DIRTY” in black text, and the removable OSHA approved “Biohazard Label” adhesive backing.
Teamwork
“Each member must be able to produce the work tasks required of their position/role,” said DeMeo. “However, each person and technician will have both innate and learned skills and attributes, and equally differing levels of strengths and weaknesses. Leaders must be able to build a team that can function effectively and as naturally as possible. If you force a process it will likely fail. I have found that it helps to implement human factors elements or human factors engineering principles in addition to general CS/SPD necessities.”
Collaboration
Because the actions of the OR directly impact the CS/SPD and its ability to turn around instruments quickly, effectively and safely, there must be close collaboration between the two“It is not so much about how the CS/SPD can improve efficiency, but how everyone else, particularly the OR, impact the process,” said Sargent.
Sargent recently conducted a hospital assessment and found that while the CS/SPD team was performing its tasks correctly and working efficiently, the OR team was haphazard about its point-of-care cleaning. To educate both teams on their impact on one another and help overcome this issue, she recommends that hospitals implement cross training programs where OR technicians spend time in the CS/SPD, and CS/SPD technicians spend time in the OR.
Sargent says another key stakeholder in promoting the reprocessing of clean and safe instrumentation is infection control.
“It is really a three-legged stool: CS/SPD, infection control and the OR,” said Sargent. “These parties should come together, review the AAMI standards and AORN guidelines to find out what they are doing right and where they have opportunities, then put together a strategic plan for improvements.”
Data
Documentation
DeFee says effective documentation is a key factor in the success of his department, stating:
“I’ve been through four or five state inspections and one of the factors that the inspectors find most impressive about our department is the level of documentation,” said DeFee. “If someone on our team is looking for information to do their job they are able to easily find it. I am also sure to continuously update team members on changing standards that impact their work.”
Standardization
“Take the example of routine sterilizer load release,” Flynn added. “Many facilities have adopted the best practice of monitoring every sterilization load, whether steam, EO or VH2O2, with a biological indicator (BI). The standardized workflow is to release load items only after they are cool (for steam-processed items) and all quality control results, including the BI result, are acceptable. Adopting this standardized workflow can simplify staff training, improve quality, and reduce the need for rework.”
Instrument tracking
Finding ways to efficiently process instruments is obviously a tremendous challenge — but what if you can’t find the instrument to begin with? Missing or lost instruments is a major source of frustration and delays — in the OR and CS/SPD.
“I see the issue of missing/lost instruments as being an area most in need of improvement and is, in my opinion, the largest obstacle to workflow efficiency in a CS/SPD,” said Todd Schojan, Laboratory Coordinator at Highpower Validation Testing & Lab Services. “When an instrument is missing it can cause set down time, re-work and the biggest obstacle to efficiency — CS/SPD staff spending hours looking for an instrument if it is doctor-specific or one of a kind. Missing instruments have the potential to render a tray useless and can wreak havoc. They can cause case delay, rescheduling and even cancellation, leading to frustration not only to CS/SPD and OR staff but to the surgeon and the patient as well.”
“There is no substitute for staff diligence and solid standard operating procedures to ensure that each instrument is accounted for and stays with the set it belongs to,” added Schojan. “However, instrument-level tracking systems can help to keep instruments from going missing, or at least greatly reduce the time it takes to find ones when they do. RFID tags in conjunction with tracking systems can help staff locate instruments in real time and greatly reduce money spent on replacing lost instruments.”
Special considerations
While the best practices highlighted in this article apply to most instruments flowing through the CS/SPD, some items present unique challenges when it comes to reprocessing efficiency.
Robotic instruments
Loaner trays
The delivery of loaner trays, and the condition in which they arrive at the facility, can make or break the reprocessing workflow. Mary K. Lane, MHA, CSPDM, CSPDS, CSPDT, MK Lane SPD Consulting, offers her advice on boosting efficiency in this area.
“The CS/SPD must implement a firm policy for vendors with surgeon buy-in that encompasses receipt to the pick up of the trays,” said Lane. “Vendors are expected to have their trays to us not later than 24 hours prior to the surgery time, which is gracious on our part. Failure to do so means the vendor has to provide a written explanation and the surgeon is notified that they might encounter a surgical delay because of the late vendor trays. A repeat offense within 14 days results in a letter to the vendor advising them that if they are late a third time they are on a 30-day suspension from the hospital. Subsequent infractions result in more severe consequences, up to being banned from the hospital.”
References
1. https://www.ahrq.gov/news/newsletters/e-newsletter/503.html
2. Use of A Novel Sterilization Process for Surgical Instruments, 2019 Association of periOperative Registered Nurses (AORN) Global Surgical Conference & Expo
About the Author
Kara Nadeau
Senior Contributing Editor
Kara Nadeau is Sterile Processing Editor for Healthcare Purchasing News.