The full scope of reprocessing: Introspection and intervention
When does the reprocessing of endoscopic – or any medical/surgical – device or instrument really begin?
To the layperson, outside observer or even patient, that process begins in the Sterile Processing and Distribution (SPD) department, right?
Nope.
It’s in the Operating Room (OR) department, specifically the Surgical Suite just outside the sterile field where the patient lies.
Ironically, and tragically, as the reprocessing process technically starts there, so do the problems, which unfortunately cascade through the rest of the process in a domino effect.
Hopefully, few within healthcare – even outside of SPD and the OR – would be naïve enough to oversimplify the sterile reprocessing process by comparing it to the stereotypical diner/restaurant operation of clearing and cleaning tables and then running the dishes and utensils through the sonic washer in the scullery. In fact, it’s way more complex and involved than that – and for good reason: The chance and prospect of contracting a deadly infection generally is more prevalent in a healthcare facility setting than in a diner/restaurant.
Based on more than four decades of Central Service/SPD editorial coverage, Healthcare Purchasing News generally categorized the reprocessing of endoscopes into 10 distinct segments that could function as progressive steps along the way. They are:
- Pre-cleaning and treating
- Leak testing
- Manual vs. automated cleaning
- Visual inspection techniques and technology
- Cleaning verification testing
- HLD and rinsing
- Sterilization and aeration
- Drying
- Storage and handling
- Maintenance and repair
HPN then reached out to more than three dozen executives and professionals from providers, suppliers and service companies in a mammoth, but monumental exercise: Examine each step, identify specifically what and where are the weakest link(s) where mistakes most commonly are made, listing what can or will go wrong and why, followed by what SPD can and should do to solve the problem.
Through her team’s comprehensive research Ofstead has pinpointed a number of potholes and roadblocks in the 10 steps of SPD operations.
“For all of these steps, the most common breaches we’ve observed during audits and research site visits involve a failure to do critically important steps at all or cutting corners in ways that undermine reprocessing effectiveness,” Ofstead told HPN. “This is generally due to a combination of three things: Lack of sufficient training, lack of adequate time and resources for the scopes used at the facility and lack of support and accountability.”
Last year, Ofstead and her team collaborated with IAHCSMM on a survey about endoscope reprocessing, generating a response rate that exceeded 2,300 SPD professionals. Several themes stood, out, according to Ofstead:
- 72 percent received less than a week of training, and 25 percent received no training or only one day of training before being expected to reprocess endoscopes independently
- 31 percent said they can’t understand the manufacturers’ IFU for endoscopes
- 34 percent said that it’s not feasible to follow the reprocessing IFU
- 70 percent said they are under pressure to go faster when reprocessing scopes
“Fixing the problems will require a substantial investment of time, training and other resources,” Ofstead asserted. “A major challenge for SPD will be the need to demonstrate a business case for making these investments. To succeed at quality improvement will require active collaboration with other departments that use endoscopes or are responsible for patient safety, including perioperative and endoscopy services, ER/ICU, infection prevention and risk management.
“To sustain quality improvement, facilities should regularly ask for input from front-line personnel and provide feedback on adherence and outcomes to the techs, their supervisors and other stakeholders, including infection prevention, perioperative services, and risk management,” she encouraged. Ofstead recently published the findings of several studies related to these issues that are accessible via her company’s and IAHCSMM’s web sites.
What follows is a state-of-the-industry professional assessment of the reprocessing process by experts in their own words.
Pre-cleaning and treating weak links
Stephen Spanos, Medical Director, Ambu Inc.: “Compliance: With much of this process, much of the success of the cleaning process depends on the compliance of the staff responsible for cleaning. Given a busy procedure room or low staffing during nights and weekends it is possible for the pre-cleaning to be missed entirely.”
Shaun Sweeney, Vice President, Cygnus Medical: “It’s very troubling to see how many facilities still skip the first step of bedside cleaning. This step removes the largest amount of gross contamination and is essential in achieving high-level disinfection. Often staff members will assume that because the scope will soon be soaked and brushed that it is not necessary to flush the channels at bedside. When this step is skipped it compromises all the cleaning stages that follow.”
John Whelan, R.N., Clinical Education Coordinator, Healthmark Industries: “Not uncommon gaps in flexible endoscope precleaning practice involve completely skipping pre-cleaning, or not doing it completely or correctly. Additionally, incomplete communication [regarding] pre-cleaning time affects the processing steps to follow. Incorrect or absent pre-cleaning allows for development of harmful biofilm and makes the removal of residual bioburden that much more difficult. Pre-cleaning needs to occur as soon as the endoscopy procedure is complete – by procedure staff. Minutes matter. The time of pre-cleaning needs to be effectively communicated by clinicians to reprocessing staff so that (when needed) extended soaking/cleaning can occur as prescribed by endoscope manufacturers’ Instructions For Use (IFU). Not communicating this information clearly handicaps the staff responsible for the manual cleaning steps.”
Crit Fisher, Director, Onsite Service & Operations, KARL STORZ Endoscopy-America Inc.: “Pre-cleaning is the most overlooked or omitted process in the decontamination and reprocessing of flexible and rigid endoscopes.”
“Endoscope use within the operating room presents a unique challenge to expedient reprocessing. Often, the endoscope may be used and set aside for large portions of the case. Delay in cleaning has many of the same effect as not cleaning the scope at all.
“For gastroenterology procedures, the most often missed step remains the installation and use of air/water channel cleaning adapters for applicable models. This step is awkward and often causes water to spurt from the cylinder after removing the air/water button when the air pump is engaged. Also noteworthy is the additional flushing of auxiliary, balloon and elevator wire channels. The lack of properly cleaning ancillary channels greatly increases the risk of an adverse event.
“Adding to infection control concerns, even with cleaning between uses, many towers are unintentionally contaminated. Handling soiled endoscopes while performing insertion tube wipe down, suctioning and flushing risks the spreading of contaminants to equipment and accessories on the tower. Be sure to handle ‘reusable’ items on the tower, such as the water bottle tubing, flushing pump tubing and pigtail as clean elements and do not cross-handle these items after handling with contaminated gloves. These items will be reattached and used with the day’s remaining patients and it is impossible to be sure there was effective low-level disinfection of all mated surfaces or crevices.”
Cori Ofstead, President and CEO, Ofstead & Associates: “Often the clinicians and personnel in the OR, ER, ICU, etc., assume all reprocessing is taken care of in Central Sterile, and they do not appreciate the need to remove soil at the point of care, so they skip this step. We’ve also seen cases where certain aspects of pre-cleaning are skipped — like failing to wipe down the surfaces or flush the channel before transport. Sometimes the patient care unit doesn’t have pre-cleaning supplies, while other times their staff haven’t received training in this critical role. This is especially true when scopes are used in the OR, ER, or ICU after hours for emergency cases.”
“Not using correct accessories/adapters (per endoscope OEM’s IFU) to perform pre-cleaning: Failure to use cleaning accessories may prohibit correct pre-cleaning of some internal channels/surfaces of the endoscope.
“Not performing pre-cleaning as soon as possible after the procedure – ideally, pre-cleaning is performed as soon as the endoscope is removed from the patient: Allows soils and bioburden to dry on endoscope surfaces, which may make soils more difficult to remove and the endoscope more difficult to clean thoroughly.”
Christian Ezagui, CER, CST, CRCST, Technical Resource Manager, Paces MedEquip LLC: “Inadequate pre-cleaning can be a contributing factor in hospital-acquired infections (HAIs). Fast OR Room turnover with busy schedules can negatively influence the established pre-cleaning and treating protocol.”
Brian Newton, COO, Parametrik: “Pre-cleaning and treating weak links are consistency, volume and application. Both are manual processes that require education and monitoring.”
J. Hudson Garrett Jr., Ph.D., Global Chief Clinical Officer, Pentax Medical: “Time is always a critical element with the in-room pre-cleaning process. This process is critical to begin the removal of gross organic soil and bioburden.”
Jean Sargent, President, Sargent Healthcare Strategies: “Lack of knowledge: The staff who should be completing the pre-cleaning at the point of use have many responsibilities, and the focus is generally not the pre-cleaning of scopes. It is not because they don’t want to complete their responsibilities; it is that they have too many responsibilities and not enough time, therefore something may get missed. The staff at the point of use may not have received proper training which would support their understanding of their role of the first steps in the Instructions For Use (IFU).“Think of the last time that you cleaned a breakfast plate that had dried egg yolk on it. Have you noticed how much harder it is to remove the yolk depending upon how long the plate sat before cleaning began? Now consider that these same substances, protein, fat and carbohydrates are what can be on a flexible endoscope after use. When it comes to removing debris, time is of the essence. The sooner pre-cleaning begins the easier it is to remove the material in the cleaning process.
“Another weak links is the amount of time that flexible endoscopes sit before cleaning begins. In the SPD, if there is not a specialist in decontamination focused on the complex instruments (e.g., MIS, endoscopes, video equipment, robotics, power tools, etc.) and if the cases are processed in the order that they arrive, instruments can sit for hours before cleaning begins. The longer the instruments sit the greater the chance for the formation of biofilms that are extremely hard to remove.
GI endoscopy clinics are not immune to delayed cleaning if the technicians are tasked with room set-up or other tasks and if there is insufficient staffing.”
Fouad Bahout, Vice President, Sales & Marketing, Surgmed Group: “Waiting too long to pre-clean allows bioburden to dry up, making it harder to remove, rendering the disinfection or sterilization process less effective (per CDC).”
Robert Dybec, R.N., CPSN, CNOR, EMT-B, Nurse Manager, Operating Room, NYU Winthrop Hospital, for Ruhof Corp.
“This process is not always completed or done properly. Unlike Endoscopy units that are self-contained and in control of the entire course of reprocessing, other areas of the hospital perform procedures using flexible endoscopes. Operating Room, ENT, Speech Pathology, Radiation Oncology, for example. These areas rely on the SPD to reprocess their scopes. The important aspect of pre-cleaning cannot always be guaranteed.”
Pre-cleaning and treating - How to solve:
SPANOS (Ambu): “Increase staffing and training. If a hospital is willing to invest in higher number of techs as well as improved education programs it is conceivable the compliance rate will rise. Whether the process is able to reach 100 percent compliance is doubtful, however.
“Single-use [device] adoption should be a solution for all of these steps.”
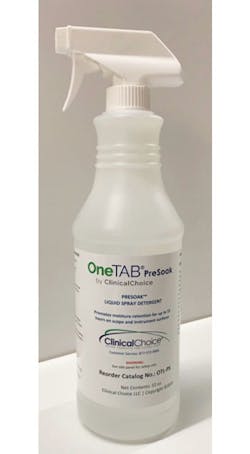
LORAN (Clinical Choice): “When pre-cleaning endoscopes, look for bedside kits with multiple detergents and sufficient liquid volume to meet OEM IFU volume requirements and to ensure fluid is clear at the end of channel flushing. Detergents should be able to clean all types of surfaces, including plastics, rubbers, optical, porous and non-porous surfaces.
“Pre-cleaning should be performed immediately after the procedure to remove as much bioburden as possible. Surgical instruments are often treated with delayed reprocessing spray. The same methodology can be used to keep endoscopes moist including the elevator mechanism area. Look for a detergent-only spray as enzymes should not be sprayed into the air. The application of a neutral pH pre-soak or delayed reprocessing spray meets OEM IFU requirements as it’s technically a continuation of wiping and channel flushing.”
SWEENEY (Cygnus): “The solution is educating the staff of the importance of bedside cleaning and having a way to monitor the process. Using ready-to-use kits offers a practical way of tracking usage and compliance. When the room is set up with proper number of kits needed that day it is easy to flag when kits are not being used.”
WHELAN (Healthmark): “Education and reinforcement for both clinical and reprocessing staff is necessary to emphasize the rationale behind pre-cleaning. Endoscopy procedures are commonly performed back-to-back so time is critical. But when staff are knowledgeable of – and respect the significance for – this step in the process, compliance is easier to maintain. Periodic ‘eyes on’ auditing of pre-cleaning practices provides further opportunity to make sure best practice is sustained.”
FISHER (KARL STORZ): “Hospitals need to understand that this is the first critical function in reprocessing, and they need to hold staff accountable to follow the pre-cleaning steps.”
VANHEE (Key Surgical): “The most effective tactic to expand your area of influence is to collaborate with your perioperative and procedural partners (OR, GI, ENT, etc.) in the creation of a point-of-use cleaning policy/procedure that includes technical training on the appropriate pre-cleaning steps according to the manufacturer’s Instructions for Use (IFU) and additional education for the procedural staff on why the pre-cleaning process has a significant impact on the subsequent reprocessing steps and helps to promote positive patient outcomes.”
KUBACH (Mobile Instrument): “Comprehensive training when new systems are installed is not enough. Regardless of experience level, staff must receive periodic continuing education as regular reminders to follow the pre-cleaning process. Special emphasis should be placed on training operating room personnel regarding pre-cleaning requirements and associated risk if it is not performed properly. This should also be included in annual competency skills and ultimately enforced by infection control auditing. When cleaning is delayed, it should be logged, and the risk assessed to avoid adverse outcomes. Additional detergent soaking will need to be performed. Some facilities notify a courier to retrieve the scope from the room once a case is completed to avoid this scenario. Timely transport reduces risk.”
OFSTEAD (Ofstead & Associates): “Three things are needed wherever reusable endoscopes are used:
- First, make sure every unit has the necessary supplies
- Second, ensure that all clinicians and staff who use reusable endoscopes are trained and competency tested in pre-cleaning (including those working at night and on weekends and holidays)
- Third, provide accountability by including an assessment of pre-cleaning adequacy in audits and communicating with involved departments about instances where pre-cleaning is not sufficient.”
BENEDICT (Olympus): “Perform pre-cleaning immediately after the procedure. Ideally, perform pre-cleaning as soon as the endoscope is removed from the patient. Perform pre-cleaning exactly as indicated in the endoscope OEM’s IFU. Do not skip steps and ensure that any required accessories/adapters are used correctly.”
NEWTON (Parametrik): “Set up periodic inservices with your staff so they understand the importance of consistency, correct detergent volumes for external surfaces and internal channels and how to apply the detergent especially when treating the endoscopes with a delayed reprocessing solution.”
GARRETT (Pentax): “Healthcare Facilities should block time in the daily schedule for ‘reprocessing activities’ that includes the total time from start to finish necessary to reprocess the flexible endoscope in accordance with the manufacturers’ reprocessing instructions for use. Currently, most healthcare facilities only track time for anesthesia services and the actual clinical procedural time. It’s critical to add a third element into our tracking efforts which is reprocessing time.”
SARGENT (Sargent Healthcare Strategies): “Create a committee to address all concerns regarding use of scopes. This committee should understand the importance of each step, the time requirements to complete each step, and include this time in the employees’ daily duties.”
AGOSTON (SpecialtyCare): “Specialization and training are the best way to ensure that pre-cleaning is properly performed for every flexible endoscope. Having a segmented specialized work force focused on complex instruments is the key. In addition, dedicated management that is expertly trained in the complex instruments assures proper training and adherence to IFUs. This limits the number of technicians/nurses that handle the flexible endoscopes and other complex instruments, making training and management easier.”
DYBEC (NYU Winthrop/Ruhof): “Random auditing of the pre-cleaning process and a practice of bi-directional tracing that includes documentation regarding the pre-cleaning process.
Leak testing weak links
LORAN (Clinical Choice): “Identifying leaks can be difficult due to time constraints and location of leaks.”
WHELAN (Healthmark): “Again, this step can be skipped if not realized as important by reprocessing staff. Leak testing for flexible endoscopes is required [for] every scope, every reprocessing cycle and before the scope is exposed to liquids. Leak testing is meant to proof for an intact device, free of leaks that could not only damage the scope (e.g., flooding and corrosion), but also allow for penetration of bioburden and biofilm that can put the patients to follow at risk. Recent experience has highlighted a need to validate the equipment used for leak testing. For years, staff were taught to ‘listen for air being discharged’ from a leak tester. This has proven to be an inadequate practice and potentially dangerous assumption. Testing of leak testers has shown insufficient or ill-sustained pressure readings. This again would put the next patients in line at risk (as well as the scope), if true leaks exist; but are not registering with the leak testing equipment. Gaps may exist within the base unit (pressure source) and/or the connection tubing. The means for proactive testing of this equipment heretofore did not exist.”
FISHER (KARL STORZ): “Leak testing is defined differently by manufacturers. This causes some confusion over when, where and how to conduct a leak test. Some manufacturers have manual leak testers, while others have automated leak testers. Add in whether the manufacturer requires a wet or dry leak test, and it’s no wonder why this step can be complicated.”
VANHEE (Key Surgical): “Leak testing is an often overlooked and underappreciated step in the flexible endoscope reprocessing cycle. The mantra that we hear in sterile processing departments around the globe is, ‘if it’s not clean, it can’t be disinfected or sterilized,’ but one important detail is left out: If a flexible endoscope is damaged, it likely can’t be effectively cleaned, and therefore can’t be disinfected or sterilized.”
KUBACH (Mobile Instrument): “Leak testing not only helps ensure a scope has not been contaminated internally but also helps guard against expensive repairs related to fluids contacting internal components. Endoscopes with leaks are not considered clean and must be pulled from patient use because the source of the leak may harbor dangerous bioburden. Extremely small leaks, especially internal leaks, escape identification until the image or internal components are damaged. Missed leaks can happen for many reasons but most are preventable.
“Common leak testing mistakes include:
- Failure to fully immerse the scope. Even the most diligent scope cleaning staff may not realize that they did not fully immerse the scope. Slow filling sinks and leaking drains result in reduced water levels that may not allow detection of leaks.
- Damaged or improperly installed waterproof caps. Scopes that require waterproof caps need to be closely examined for leaks as well. Damaged or improperly installed protective caps will allow fluid to inside the scope which can cause more severe damage. While endoscopes with caps covering electrical connection, points are designed to be fluid resistant, damaged or improperly installed caps can result in pin and contact corrosion that may affect the image.
- Immersing an unpressurized scope that fails a dry leak test. Failure to confirm the endoscope can hold safe, sufficient pressure prior to immersion can result in costly damage from fluid. Pressurizing the scope prior to any wet test submersion and maintaining insufflation while cleaning a leaking endoscope is an important factor. Special care under this scenario should be taken when utilizing a ‘hand-held’ leak tester. Maintaining safe pressure can be difficult while completing decontamination cleaning steps. Additionally, attaching or detaching leak test tubing and air displacement venting should all be done outside of the water. Failure to do so allows small amounts of fluid to slip past the O ring on the leak tester connector allowing moisture to enter the electronics, bundles and endoscope mechanics.
- Operating the scope during a leak test. Failure to sufficiently angulate the knobs during leak test or confirm all knob locks and variable stiffness adjusters are disengaged during reprocessing can cause fluid damage and the angulation system to go out of specification.
- Protecting the leak tester tubing from fluid entry. Any fluid or moisture within the tubing can be blown into the endoscope during the test. Always confirm it is dry and safely handled while working in water.
- Failure to completely vent when testing. Over pressurizing a scope without venting can cause bending rubbers to stretch due to over inflation; this can add additional risk of damage during use or reprocessing.”
OFSTEAD (Ofstead & Associates): “The most common issue we’ve observed is doing lightning-fast leak testing without taking the time to carefully inspect the scope while angulating the bending section. Other common breaches include using warm sudsy water or failing to do leak testing at all in an effort to complete reprocessing more quickly.”
BENEDICT (Olympus):
- “Leak test not being performed
- Incorrect leak tester is being utilized
- Leakage tester is not tested for functionality prior to use
- Leak test cable is attached with wet connector (pressure forces water into ETO valve)
- Leakage tester is connected to scope while under water
- Not allowing scope to fully pressurize before completing leak test
“Why it’s a problem:
- Any deviation from the Leak Testing process, or missing any of the OEM specified Leak Testing steps, subjects the device to the potential of fluid invasion and costly repair.
- Repairs can negatively affect your facilities up-time, which is the use of the device to perform life-saving procedures.
- Reduced up-time reduces your facilities ability to create revenue from the use of the device that is out for repair.”
- EZAGUI (Paces MedEquip): “Inadequate leak testing can be a factor in increasing the risk of cross-contamination between patients.
“Why it’s a problem: The leak tester is unavailable, not working properly, improperly used or the leak tester user was not properly trained and signed off during a competency review.”
SARGENT (Sargent Healthcare Strategies): “Lack of understanding and/or equipment. Staff in CSPD are asked to complete several tasks and to complete them all appropriately. There are often competing priorities and this step may be skipped due to constraints.”
AGOSTON (SpecialtyCare): “Every OEM recommends leak testing for their flexible endoscopes prior to manual cleaning. This is done primarily to detect if leaks are present so that the endoscope is not flooded with water or enzymatic solution during the cleaning process. The OEMs stress the importance of performing the testing correctly, whether it is a dry leak test or wet leak test. If the endoscope leaks, it should be returned to the OEM for repair.
“In reality, there are several weak links in the leak testing of flexible endoscopes, some identified and some that should be recognized and corrected. First, it is critically important to avoid flooding the endoscope during the cleaning process. Flooding can increase the cost of repair by tens of thousands of dollars. Second, a leaking endoscope is not safe for patient use as there is the possibility of harmful substances or organisms leaking out into the patient and by definition a leaking endoscope cannot be considered sterile or HLD. It is estimated that 70 percent+ of the returned flexible endoscopes are returned due to a leak. The majority of these leaks occur during use and cleaning.
“There are three basic systems in all flexible endoscopes, the image system responsible for transmitting the image, the mechanical system and the hermetic seal, which prevents fluid from invading the interior of the endoscope. Physicians during a procedure can only detect issues with the image and mechanical system. Unless a hole develops that is visible, which in the majority of cases holes are not visible, the physician has no way of knowing if the endoscope is leaking. Conversely, in the processing department, the test that is called for in the IFU is a leak test. This gap in knowledge (physician – video/ mechanical), technician (leak), creates a risk for the patient as today there is not a standard or regulation that requires the technician to report to the physician if a leak is found in a flexible endoscope that was just used on a patient. Recall that sterilization or HLD is only validated for the exterior of the endoscope and the interior of the lumens. The interior of the endoscope is not accessible to the user and cannot be considered clean, sterile or HDL. Thus, at the moment a leak develops in the hermetic seal of the endoscope, the endoscope must be considered non-HDL or sterile and is not safe for patient use.
“The process of sterilization or HLD only affects the exterior of the endoscope and the interior of the lumens. For some small diameter endoscopes that are sterilized by gas or plasma, a pressure relief cap is required during sterilization to allow for the equalization of pressure during sterilization. If the pressure relief cap was not installed, there is a chance that the endoscope would rupture due to the difference in the exterior and interior pressure during sterilization. While the interior of the endoscope is exposed to sterilant via the pressure relief cap, the interior of the endoscope cannot be considered sterile because there is no user access to clean and validate cleaning prior to sterilization.
“Given that a leaking endoscope cannot be considered sterile or HLD, let’s compare and contrast what happens when a general instrument or instrument container is found in the OR with debris. If an instrument or container is discovered in the OR with debris, all instruments and equipment that could have come into contact with the contaminated instrument are removed from the room. new instruments are brought to the room, and there is documentation of the patient exposure to a dirty instrument. The patient will likely be monitored closely for any signs of infection.
“In the case of the flexible endoscope, because discovery of the leak occurs after the procedure, all that is required is to return the flexible endoscope for repair. No physician notification is required by any standard or regulation at this time. While MIS procedures have lower risk for SSI, the risk is not zero, and given the growing virulence and antibiotic resistance, everything must be done to protect the patient from exposure to non-sterile/ non-HLD equipment. AAMI is currently considering adding a requirement for physician notification of leaks to ST-91. SGNA, AORN, IAHCSMM, etc. and all regulatory agencies should support and adopt this change.
“Every day across the world, flexible endoscopes are used on patients that have leaks in them, potentially allowing patients body fluids to enter the endoscope and leaching out of the endoscope substances and organisms that could be potentially harmful to the patient. Because there is not a requirement to report to the physician or record the incidences of leaking endoscopes that were used on a patient, there is no database to support an increased risk. However, by definition we know that the use of non-sterile/non-HLD instruments does significantly increase the risk of SSI. Another way of viewing this is that no technician would process, or physician knowingly use on a patient a leaking flexible endoscope. The use of leaking flexible endoscopes occurs because:
- The leak test was not performed properly,
- The leak tester was faulty,
- Damage occurred to the endoscope post leak test by the technician during the cleaning process,
- The endoscope’s hermetic seal failed due to age/ exposure to the cleaning process,
- Damage occurred to the endoscope during use to cause a leak, (contact with other devices or surfaces that caused a cut or hole, laser damage, damage from accessory instruments such as biopsy forceps etc.
“Unfortunately, OEMs and repair facilities know that some leaking flexible endoscopes are reprocessed many times and presumably used on multiple patients before being returned for repair. This they know by the amount of corrosion and contamination found inside these endoscopes when disassembled during the repair process. This is very alarming, yet because there is not a requirement or standard currently for physician notification, there is no data on the consequences of this exposure for the patient.
“This is basically the reason that leak testing is done – to prevent patient exposure to potentially harmful substances or organisms. The weak link is that the current protocol at most hospitals and clinics, and current regulations and standards do not require physician notification and documentation. Today, when a leaking endoscope is discovered after use, the only instructions for the technician in the IFU, regulations and standards is to prepare and return the endoscope for repair.
“The fault is not connecting the endoscope with the possible leak and that was not HDL or sterile from the point in time when the hole developed to the patient on which the endoscope was just used. Notifying the physician of this is important. Should the patient have any adverse reactions or events related to the procedure this information could be very valuable to the physician in the treatment of the patient. Additionally, having record of the patients who could have been exposed to a leaking endoscope is valuable information that could be used to study to see if there is a higher risk for SSI or other complications. AAMI’s committee, ST-91 is currently considering changing the guidelines to include physician notification when a leaking endoscope is discovered.
“The other weak link is that leak testing is performed before the cleaning process for both manual and automated processes. If the endoscope is damaged during the cleaning process and develops a leak, there is a chance that the endoscope will be used on a subsequent patient.”
BAHOUT (Surgmed): “One weak link is bypassing steps during leak testing or failure to follow steps in their proper sequence can result in an erroneous reading leaving a leak undetected. Another weak link is not performing a leak test daily. A leak can occur at any time and can be easily missed if not checked every day.”
Leak testing - How to solve:
LORAN (Clinical Choice): “The best way to identify leaks is by submersing endoscopes in their entirety using an automated device with continuous air. Proper staff training and sufficient time of at least two submersed minutes after channels are flushed with water will help better identify leaks. A water gun is a great tool to quickly flush water through the channels and disperse air bubbles on the endoscope.”
FISHER (KARL STORZ): “Have the IFUs posted. Conduct regular training of the leak test procedure.”
VANHEE (Key Surgical): “Leak testing is one of the best methods to detect damage that cannot be seen during visual inspection. Ensuring that leak testing is being performed with the appropriate equipment and attention to detail, on every flexible endoscope, every time, will not only prevent non-cleanable, non-disinfectable, non-sterilizable scopes from patient use, it will also help to identify damage early and reduce catastrophic repair costs.”
KUBACH (Mobile Instrument): “Effective leak testing and safe cleaning of leaking endoscopes relies heavily on following the manufacturers’ IFUs. IFU compliance should be supported with individual training with clear specific procedure or work instruction. Leak testing skills should be closely assessed during employee return demonstrations. Dedicated extended leak test time should be considered to assist with small leak identification. Test conditions should be adequate, such as recommended sink size and good illumination for visualization.”
OFSTEAD (Ofstead & Associates): “A first step is to make sure technicians understand why leak testing is necessary and how to do it properly for each type of scope. It may be necessary to automate the process or allocate a certain amount of time that should be devoted to leak testing.”
BENEDICT (Olympus): “Request frequent and documented observation and training by your OEM equipment and service provider to ensure Leak Testing is performed in accordance with their specifications.
- “Allow your OEM equipment and service provider to offer access to their on-line support materials and educational items.
- Schedule your staff to attend area educational training sessions sponsored by your OEM equipment and service provider.
- Allow your staff wall space to post OEM Leak Testing specifications and training materials to refer to during reprocessing.
- Ensure your staff fully understands the importance of Leak Testing and the costly effects of Fluid Invasion device repairs.
- Have your staff prepared to reprocess a leaking scope per your OEM equipment and service providers specifications.”
EZAGUI (Paces MedEquip): “The goal of a leak test is to detect damage to the exterior or interior of the endoscope that will cause fluid to leak into sections of the endoscope and contaminate the endoscope. Endoscopes should be leak-tested in accordance with the manufacturer’s IFU prior to immersion in any fluids. A leak-test failure indicates that a channel is perforated, torn or twisted. If this occurs, the endoscope must be tagged for repair, and the endoscope manufacturer’s guidelines must be followed while it is cleaned, decontaminated and returned to the repair facility (IAHCSMM Endoscope, 2017, p. [Page 84-85]).”
GARRETT (Pentax): “Users should carefully follow the reprocessing instructions for use and also have adequate reprocessing facilities to properly manage the flow of the endoscopes thru the reprocessing process.”
SARGENT (Sargent Healthcare Strategies): “Educate the staff in the importance of each step and missing a step may lead to a negative outcome for the patient.”
AGOSTON (SpecialtyCare): “This weak link is solved through competent technicians correctly performing the leak test per the IFU for every endoscope. In addition, we need all standards and regulations changed to state that if a leak is found in a flexible endoscope, the physician must be notified, the patient’s record modified to note the exposure, and the endoscope removed from use and returned for repair.”
BAHOUT (Surgmed): “Make sure to closely follow an endoscope’s manufacturer's recommended sequence of steps for leak testing. Leak tests should be done after each use (AORN) to confirm that the device is intact and functioning properly.”
Manual vs. automated cleaning weak links
SPANOS (Ambu): “Inadequate cleaning: Multiple peer-reviewed studies have shown that regardless of the cleaning method, reusable endoscopes are unable to be reliably cleaned. Invariably a certain percentage of ready-for-use scopes test positive for bacterial cultures. The problem lies with the cleaning process itself as channeled scopes create a unique problem in which certain components along with accumulation of biofilm prevent adequate cleaning despite adherence to manufacturers’ guidelines.
“It is also important to remember the cleaning process often involves over 100 steps, which lends significant opportunity for error. If an institution needs to choose between automatic and manual reprocessing, then automatic is preferred as it reduces the number of manual steps and theoretically reduces the opportunities for error.”
LORAN (Clinical Choice): “OEM IFUs can be complex and difficult especially if it’s not your full-time job. Pressure to turn scopes around quickly can increase the risk of missing one of the required cleaning steps.
“Similar to pre-cleaning, detergents used in manual cleaning vary in quality and effectiveness. Storage, transport and usage temperatures and shelf life can degrade enzyme and cleaning capability. Exceeding transport, storage and usage temperatures creates noncompliance and may decrease cleaning effectiveness. Liquid detergents need to be measured and dispensed according to the concentration and water volume. Dispensing of liquid detergents can be inconsistent due the manual or automated pump. Enzymes effectiveness in liquid detergents can degrade over time as formulas vary by manufacturer.”
WHELAN (Healthmark): “Published research has highlighted the steps of manual cleaning for flexible endoscopes as numerous, labor intensive and highly prone to human error. Manual cleaning is the most important step in reprocessing as residual bioburden or biofilm can render disinfection/sterilization incomplete. Automated processes can allow a higher degree of consistency and standardization, but with current technology available at the sink lane only automated detergent delivery, flushing and suctioning are available to supplement the otherwise manual processes of washing and brushing. Correct and effective cleaning needs to include the use of lint-free cloths or sponges and brushes that meet channel size specifications. Risk exists when staff or management otherwise arbitrarily choose cleaning supplies that do not meet these requirements. Also, maintenance and QC for automated cleaning equipment must be performed – as per those manufacturer IFUs – to insure consistent and safe process steps.”
FISHER (KARL STORZ): “This has been an ongoing debate as manufacturers have a wide variety of steps and methods within the IFUs to address manual and automated cleaning. All manufacturers support and list a manual cleaning method in their IFUs or cleaning and reprocessing instructions. The biggest issue comes with the automated cleaners. As manufacturers take a product to market, the FDA requires them to have a 510(k). Not all manufacturers have an automated cleaning option due to the validation required. Add that there are many different types of automated cleaning units out in the market, and this can be confusing. Where manufacturers support both, I believe that both manual and automated cleaning provides the best solution for patient safety.”
VANHEE (Key Surgical): “Over the past several years, automated cleaning of flexible endoscopes has been somewhat of a hot topic and the center of many endoscope decontamination debates. Understandably so, the FDA cleared automated cleaning claims of several automated endoscope reprocessors (AER) have been both praised and vilified in the sterile processing industry. Should these automated cleaning cycles entirely replace the manual cleaning process at the sink? The short answer is: No.”
KUBACH (Mobile Instrument): “With the current infection climate most facilities are performing all manual cleaning steps even if their facility has automated endoscope reprocessing units that have advanced cleaning claims that allow the elimination of specific cleaning steps. This double effort is also supported by most recommending organizations and national standards.
“Manual cleaning means physical human cleaning so there are several things that may slightly vary or be performed at a higher level of efficacy from one individual to another. The use of lint-free sponges and cloths has greatly improved residual fibers left within and on the equipment. Different models of endoscopes may have a vast difference in channel size and use of an incorrect size brush can result in poor cleaning contact within the channel.
“Strict adherence to update IFUs for duodenoscope reprocessing is a must, and required secondary specialty brushes must be ordered from the equipment OEM.
“Most of the gastroenterology and airway endoscope models require cleaning adapter use and 30 seconds of suctioning. This is the most often missed step due to many departments lack of suction access. This step is a retrograde suction step that is often ignored and justified with additional flushing. These steps move fluids through the endoscope in opposite directions so one does not have equal cleaning benefit to the other, and they should not be interchanged or dismissed as repetitive.
“Reprocessing personnel need to understand the features of their surfactant-based detergent or enzymatic detergent to get optimal performance from their chemical. The ratio of water to chemical dosage, temperature use parameters and contact time should be observed. Many departments count the overall time the endoscope was in the sink as contact. It is actually not counted until all gross debris is removed externally, internally, and until channels are sated. Often the dedicated chemical contact time soak that occurs after brushing and flushing is not observed, and the chemical cleaning benefit is not realized.
“Eliminating use of required cleaning adapters or utilizing syringes to flush directly into ports that were not designed for syringe use should be corrected. Syringes that are not the recommended size designated by the manufacturer are not going to deliver the validated pressure or volume. The lack of cleaning adapters and tubing would effectively render the endoscope soiled.
“Many departments utilize flushing units to increase flushing volumes and reduce repetitive motion injuries. Flushing units and their hook-ups need to be quality checked and decontaminated per the IFU, usually daily. Failure to complete this may result in inadequate flushing and even increased risk of developing biofilm within the hook-ups and even in the unit itself. Minimum flushing volumes can be exceeded but the volume recommended by the manufacturer for each model should never be lessened.
“Inadequate rinsing removal of all residual detergent prior to manual high-level disinfection may cause poor chemical contact and ineffective disinfection.
“Proper brushing and flushing of all lumen devices, such as Savory dilators have historically been remiss. Reusable esophageal dilators that undergo high-level disinfection should be treated no differently than an endoscope.
“Decontamination sinks are often not sanitized and cleaned between uses, which can increase bacterial levels in the cleaning water.”
OFSTEAD (Ofstead & Associates): “Most of the issues we’ve observed are related to time pressure or a lack of training or visual cues for critical steps, such as:
- Failure to clean the channels and ports at all
- Failure to scrub the outside of the scope
- Improper dilution of detergent
- Lack of water temperature management (often too cold)
- Use of brushes that are too big or too small for particular scopes
- Cutting corners to save time and effort through inadequate soak time; advancing the brush through the channel one time as rapidly as possible, rather than brushing thoroughly; insufficient rinsing, which leaves soil and detergent residue on the scope.”
EZAGUI (Paces MedEquip): “With manual cleaning, having the correct amount of enzymatic and water at the correct temperature, per the enzymatic manufacturer’s recommendation, are mixed to create the cleaning solution. Enzymes may be less effective in removing debris if the temperature or concentration of the solution is not correct. (IAHCSMM Endoscope, 2017, p. [Page 184-185]).”
“Manual cleaning requires the technician to perform all steps suggested by the manufacturer IFU to be executed exactly as stated every time no deviations. Some scopes have many steps to be performed, and all the scopes can have slightly different cleaning protocols. This is a very large constraint to overcome in endoscopy labs. (IAHCSMM Endoscope, 2017, p. [Page 184-185]).”
NEWTON (Parametrik): “Following the OEM IFU manual cleaning instructions can be tedious and time consuming. Dedicated staff typically does a better job in following IFU details.
“A major weak link in manual cleaning is that it’s a manual process. All of us make errors and unfortunately, if an important step is missed in the manual cleaning process, it can handicap endoscopes from reaching full high-level disinfection or sterilization.
“The FDA has cleared a small number of AERs to replace manual cleaning with automated cleaning. Unfortunately, the market is hesitant to utilize automated cleaning cycles due to conflicts in societal guidelines and additional time associated with the cycle.”
GARRETT (Pentax): “Human error is always a potential risk when manual, human-driven processes are being utilized.”
AGOSTON (SpecialtyCare): “Manual cleaning must always be performed before automated cleaning. To be successful, technicians should follow all instructions in the IFU and follow them in order. QC checks and verification should be used to ensure that the IFUs are always followed. This could include the use of video surveillance and software document that IFU were followed. In addition, testing for ATP or protein in the most challenging areas to clean (lumens) is a good practice and should be performed on every endoscope cleaned. Any endoscope that fails these tests should be cleaned again.
“Borescopes are another useful tool as a weak link in cleaning is in the ability of the technician to visualize the interior of lumens. A borescope is a great tool for this.
“For Automated cleaning via an Automated Endoscope Reprocessor (AER) it is extremely important that the technician follow all IFU for the AER. The connection of the AER hoses to the endoscope is an important step as is validation that the correct chemicals are available, at the proper concentration and not expired. Filters must also be checked and changed as needed. Advantages of automated cleaning are that it is timed, recorded and standardized for all endoscopes processed. Manual cleaning generally does not have these advantages but it does have the skills of the technician and the technician’s ability to visually inspect the endoscope, which AER cannot do.”
DYBEC (NYU Winthrop/Ruhof): “Manual cleaning with its many and varied steps could result in complacency by cleaning staff – cutting corners to save time.”
Manual vs. automated cleaning - How to solve:
SPANOS (Ambu): “There is no good solution for better cleaning. No cleaning technique has been shown to provide 100 percent sterile scopes every time. We advocate transition to single-use scopes for the problems listed.”
LORAN (Clinical Choice): “Cleaning technicians should be certified, inserviced and tested periodically to ensure the best cleaning results. They should also be rewarded with pay commensurate to other important reprocessing positions.
“Utilize cleaning detergents that contain multiple detergents and multiple enzymes to maximize cleaning efficiency. Double-check the detergent technical data sheet for storage and usage temperatures. For example, one popular cleaning detergent is to be stored below 90°F with not to exceed usage temperatures of 130°F. Utilize products with storage and usage temperatures that create compliance and best cleaning effectiveness.
“When dispensing liquid detergents manually, measure the amount of detergent and the volume of water in the sink. The manual pump may not always dispense the same amount each time, and pumps can be geared to dispense different volumes, typically ½ to 1 ounce. Automated pumps should be periodically checked as they too can inconsistently dispense the wrong dosage. Incorrect dosing is non-compliant and can reduce cleaning effectiveness.
“Check with your detergent manufacturer for potential decreases in enzyme effectiveness over time and try to use liquid detergents well before their expiration date.
“The best way to compare and test cleaning effectiveness is to measure and track performance post manual cleaning. Powdered detergents with better storage and usage temperatures and wide ranges of water volumes are an excellent solution to variables associated with liquid detergents.”
WHELAN (Healthmark): “Management needs to insure adequate focus on training and competency – initially and ongoing. This cannot be emphasized enough. We need to make sure staff begin with best practice and maintain that standard practice on an ongoing basis. Similarly, ‘at the elbow’ supervision and support are critical to monitor, support and sustain effective cleaning. Periodic inventory reviews are critical to ensure the equipment and supplies used in cleaning match the specifications for the current inventory of flexible endoscopes, as well as current standards and guidelines. Processes need to be in place to insure timely and appropriate maintenance and QC for automated equipment.”
FISHER (KARL STORZ): “This is a stretch. I believe that there should be a national standard that all manufacturers must adhere to that has similar steps for manual cleaning. Manufacturers should all determine the best form of automated cleaning, and that should be the standard. Having the same standard across all manufacturers could alleviate ambiguity or confusion.”
VANHEE (Key Surgical): “Automated cleaning cycles can add a powerful additional cleaning step after manual cleaning, flushing and rinsing at the sink and should be used in that fashion. The mechanical cleaning action of brushing at the sink is vital to clinical soil removal, and disruption of mature microbial biofilms and should be performed on every scope, every time. If your facility has the capability of running an automated cleaning cycle in your AER, take advantage of the incredible benefits it provides, in addition to the manual cleaning steps performed at the sink.”
KUBACH (Mobile Instrument): “Manual cleaning should be supported with training, procedure, auditing and competency. The manufacturers’ instructions for use should be reviewed annually for each flexible model type. Chemical and cleaning aid devices should also have manufacturer support for install training and periodic review. All accessories and environmental cleaning should be clearly established and understood. Cleaning areas should include support for all steps to be completed which should easily be identified and corrected during gap auditing.”
OFSTEAD (Ofstead & Associates): “Training and visual cues; automation of as much of the process as possible, including detergent dilution, temperature management, and irrigation pumps for flushing and rinsing; and accountability provided by co-workers, supervisors and auditors.”
DANIELS (Olympus): “Follow manual cleaning steps described in the IFUs; utilize a flushing pump, according to IFUs from manufacturers when you replace pumping with syringes; use documentation/tracking systems to ensure all steps are completed.”
EZAGUI (Paces MedEquip): “Automated washing provides the following benefit. Automated was cycles are consistent, timed and documented. There is no variability with times and processes between loads, which cannot be said for hand washing. (IAHCSMM Endoscope, 2017, p. [Page 184-185]).”
NEWTON (Parametrik): “Require reprocessing certifications and hire full-time staff dedicated to manual cleaning. Perform periodic education and training to ensure there is a knowledge base across endoscope types as cleaning instructions may change by model. It’s also important to check cleaning performance. At a minimum, endoscopes should be randomly checked. Checking after every manual clean guarantees the best performance. Last, but not least, pay your technicians well. Above-grade pay helps retain staff and their skillsets. It’s also a great performance incentive.
Although worst-case scenario events should not occur in the real world, both endoscope and AER manufacturers are required to meet the same FDA cleaning requirements. Therefore, AER automated cleaning achieves the same level of clean achieved by manual cleaning if following every step of the IFU. Check with your AER manufacturer on their cleaning claims prior to use. Claims may vary by manufacturer.
“AER manufacturer automated cleaning claims have been cleared at 6.4 or less micrograms of residual protein. One AER company is cleared at 3.7 micrograms of protein also under worst-case scenario testing.”
GARRETT (Pentax): “Users should be properly trained by the endoscope manufacturer on the appropriate reprocessing instructions for use and then observed for competency in performing the process independently. Users should also receive frequently training updates by super-users within the healthcare facility and/or the endoscope manufacturer to assist with maintaining competency in the process. If automated, validated, cleaning and reprocessing processes are available, they should be evaluated for efficacy and reliability, and utilized when possible to reduce human error.”
AGOSTON (SpecialtyCare): “Technician training is extremely important as is QC checks and competency evaluations.”
DYBEC (NYU Winthrop/Ruhof): “Cleaning staff should have yearly competencies, continual training and updates on new IFUs, policies and procedures. Random audits on staff doing manual cleaning should be performed also.”
Visual inspection techniques and technology weak links
James Schneiter, Founder, America’s MedSource Inc. “Microscopic bioburden and biofilm is invisible to the human eye making the task physically impossible.”
LORAN: “Primary weak links are training, time/space and equipment to best identify opportunities.”
WHELAN: “Basic visual inspection should occur at every step along the way by clinical staff pre- and post-procedure, through all the steps of reprocessing, through storage, and back to clinical use again. However, it is also a distinct step in reprocessing that immediately follows manual cleaning. As SGNA states, this is a purposeful ‘time out’ where assessment is made to determine whether the scope is clean enough to proceed further. Basic inspection is with the unaided eye. Investigations and research have shown that often this is not enough. The unaided eye can pick up gross debris or damage, but lighted magnification, cleaning verification testing and enhanced examination with a borescope can markedly improve the yield.
“Historically, inadequate physical space design, limited financial resources, insufficient understanding of the need to inspect or simply rushing through processes have limited the amount of inspection occurring. Several peer-reviewed articles and posters in recent years have served to increase awareness for this. Flexible endoscope reprocessing standards and guidelines are being rewritten to emphasize the significance and practice expectations for enhanced visual inspection.”
FISHER: “Borescopes have been in the limelight as of late as a way to inspect the inner lumens of endoscopes and instrumentation. The biggest missing or weakest link is the training. You have these scopes, you hook them up and pass them through. There is very little training on what to look for or what you are even looking at. Some manufacturers have designs in their working channels for functionality that – to the untrained eye – may look like an imperfection. The second area is the time that it takes to conduct these tests. Many hospitals run lean on equipment and volumes, and cases can get affected by reprocessing and sterilization delays.”
VANHEE: “Visual inspection techniques and technology have vastly improved in the recent past and will continue to improve in the fast-paced healthcare industry. Over the past several years the use of new technology, such as video magnification and high-definition borescopes as visual inspection tools has become increasingly more common in sterile processing departments across the country. Frankly, inspection tools will continue to advance at a rapid rate. However, if sterile processing professionals aren’t taking advantage of the new capabilities that are afforded by new technology, we are missing out on the opportunity to improve outcomes and reduce errors in our departments.”
KUBACH: “Adequate inspection is as required as leak testing. Examination for residual debris, deterioration or damage is often completed without the aid of adequate illumination or magnification. Damaged or bio harboring pockets can endanger the patient and hinder the cleaning process.”
OFSTEAD: “Many facilities are not doing any visual inspection at all not in CS/SPD or the endo reprocessing suite, and not at the point of care. Many facilities do not have magnifying glasses or borescopes, and technicians report they don’t know what to look for anyway.
In our recent survey of IAHCSMM members: 31 percent said that being unable to see inside scopes is one of their biggest challenges. Yet only 14 percent use a borescope to look inside endoscope ports and channels, and only 18 percent use a magnifying glass to inspect the outside of the scopes.
“When we visit sites and use lighted magnification and borescopes for visual inspection, we observe defects, debris, retained fluid, or residue in 100 percent of endoscopes at every site. CS and endo department techs may not have the authority to send scopes out for repair, which reduces their enthusiasm for careful visual inspection.
BENEDICT: “Failure to perform visual inspection of the endoscope to identify any visible damage and/or debris.”
EZAGUI: “Visual inspection of flexible endoscopes was always recognized as a ‘good idea,’ but it recent years, visual inspection of flexible endoscopes has received support from leading industry standards and guideline providers (i.e. ANSI/AAMI ST91, AORN, and SGNA).
“Insufficient training leaves endoscope reprocessing technicians struggling to perform appropriate and thorough inspections of the external and internal surfaces.”
NEWTON: “Primary weak links are issue recognition, space and time.”
GARRETT: “Visually inspecting the flexible endoscope is a frequently omitted step by users and is important in identifying any external defects and risks to the endoscope.”
AGOSTON: “The ability to visually inspect the flexible endoscope is the biggest advantage that technicians have over AERs yet, due to the fact that most flexible endoscopes have lumens, visual inspection is challenging. For this reason, borescopes are recommended as well as is testing for protein or ATP.
“Often the physical facility is a challenge in that, there is not adequate work space to lay out the flexible endoscope and inspect is thoroughly. Due to this the visual inspection is usually limited to the leak test where the technician is either observing for a fall in pressure (dry test) or looking for the formation of bubbles while the endoscopes is submerged under water (wet test).
“The technician’s skills and thoroughness are the key factors affecting the quality of the visual assessment.”
BAHOUT: “Not using a borescope for inspection of internal channels. Some hospitals tend to inspect with a borescope after the manual cleaning step but before the scopes are disinfected. The endoscopes, however, are still contaminated at this point of the process, and the internal channels are still wet.”
Visual inspection techniques and technology - How to solve:
SCHNEITER: “Until and unless a scope manufacturer designs and validates a scope that can be cleaned of all organic debris, the problem will continue to persist.”
LORAN: “Utilize in-services by OEMs and ISOs to create best-practice visual inspection techniques. Create inspection protocols and allow for sufficient time to perform inspections during operational workflow.”
WHELAN: “Minimally, the use of lighted magnification is necessary to improve practices. There exist a wide array of options and costs to choose from. Future budget planning should include adding borescopes for much improved (and/or previously unavailable) inspection of internal channels and distal ends. Reprocessing policies and protocols within the institution need to set the expectation for enhanced visual inspection. Training and competencies need to provide the framework for, and assessment of, inspection practices.”
FISHER: “More training and competencies.”
VANHEE: “With the use of borescopes, we have the opportunity to inspect areas of endoscopes that are susceptible to damage and contamination that were previously impossible to visualize.”
KUBACH: “Inspection can also be aided by utilizing borescopes, whether fiber or video, to examine the condition of internal channels. Both the visual and borescope inspection are not always completed at the correct point of the process. This should be performed after manual cleaning and prior to sterilization so that the cleaning can be completed before moving into the clean process and not adding the possibility of recontamination. An additional inspection can be completed after the endoscope is high-level disinfected only if the borescope itself has be high-level disinfected with each use. It is also not uncommon to hear reprocessing personnel express their confusion as to what they are seeing and if it is an issue that needs to be addressed.
“All types of inspection can be used as valuable verification tools. Training that shows how to assess with visual examples of damage or cleaning breaches should be provided to improve inspection accuracy and understanding. This should benefit effective pulling of defective equipment in a timely manner greatly improving patient safety.”
OFSTEAD: “Facilities can start by:
- Providing magnification systems and borescopes
- Ensuring that all technicians and supervisors have received training in how to use these tools. This may be more easily said than done! Managers could also request training from endoscope manufacturers and visual inspection system vendors.
- Allocating time for visual inspection
- Providing photos showing what scopes should look like and what defects require repair
- Provide positive reinforcement or tangible rewards for techs who identify residue requiring re-cleaning or defects requiring repair
- Ensure that all endoscopes receive preventive maintenance and that they’re sent for assessment and repair whenever there are visible defects
- Provide accountability by having a qualified person periodically inspect the entire fleet of endoscopes to ensure no defective scopes are in use.”
BENEDICT: “Ensure reprocessing technicians follow the endoscope OEM’s IFUs on how to visually inspect the endoscope for damage and/or debris.”
EZAGUI: “Visual inspection is an important part of the quality process and failure to detect endoscope damage of any soil that remains on the device following cleaning is a patient safety issue. It is important that inspection takes place in a well-lighted area. Flexible endoscopes are dark in color, and it is difficult to see blood and other body substances. Therefore, ensuring there is adequate lighting is the first step in developing good visual inspection processes and practices.
“The most important areas for inspection are the lumens that run through the endoscope. Lumens pose a cleaning challenge because of their narrow structure that prevents visualization during cleaning. Therefore, it is important to always check lumens for cleanliness after cleaning. Visual inspection of the lumens can be accomplished using a borescope, a small flexible fiberoptic device that enables visualization of otherwise inaccessible areas within endoscope lumens. This inspection step can help identify debris present inside lumens and, in some cases, may reveal damage that could otherwise go undetected (IAHCSMM Endoscope, 2017, p. [Page 111-113]).”
NEWTON: “Ask your borescope manufacturer if they have a library you can utilize to identify issues with the endoscope, or does the system utilize Artificial Intelligence (AI) to create a library? Available space and time can be limiting factors in inspection frequency. Look for systems that minimize space and quickly automate the inspection process.”
GARRETT: “Users should follow the manufacturer’s instructions for use regarding the use of magnified optics to improve visualization. If abnormalities are visualized, then the device should be removed from service and sent to the manufacturer for evaluation and repair if necessary.”
AGOSTON: “Facility improvements if necessary, accessory testing equipment and supplies, leak testers, protein/ATP tests and bore scopes along with competent technicians.”
BAHOUT: “Using a borescope to inspect internal channels is very important because according to AORN, the fact that endoscopic cameras and borescopes penetrate the lumen allows for improved visual inspection. The scopes have to be completely dry prior to inspection with a borescope or else bioburden and mostly water would interfere with this process.”
Cleaning verification testing weak links
SPANOS: “Verification testing like most of the segments in this process relies on high compliance with a manual process. Additionally, swabbing and protein analysis to determine contamination is an unreliable indicator for determination of bacterial contamination. Performing flush-brush-flush testing with associated culturing is far more accurate but will significantly increase costs and is impractical with expected scope turnaround times.”
LORAN: “Endoscopes are not always tested during reprocessing. An unclean endoscope could hamper high-level disinfection or sterilization.”
WHELAN: “Cleaning verification can be considered part of inspection in the sense that any failure requires a return to full manual cleaning. Many facilities are unclear as to what to use for, and how often to perform, cleaning verification. Cleaning verification provides a marker of cleaning adequacy. It serves the basic principle that we cannot measure/assess something we do not test for.”
FISHER: “This is one area that I am very supportive of, and, with the exception of training, find very effective in the war against hospital-acquired infections.”
VANHEE: “Cleaning verification for flexible endoscopes is a relatively new area of interest. Many cleaning verification modalities have been explored and commercialized over the last several years, many of them originating from the food safety and hygiene industry. The challenge that we face in the sterile processing industry is the lack of standardization in cleaning verification testing.”
KUBACH: “Cleaning surveillance testing by using organics or ATP can provide valuable information that cannot be detected with the unaided eye. Testing can also be used as verification of effective reprocessing but should be done at the end of decontamination. Using these tests out of order can hinder test results that may provide indicators of cleaning process gaps and need or retraining.”
OFSTEAD: “Most sites are not yet doing any biochemical tests to verify cleaning effectiveness. Sites that are doing some kind of testing are generally doing it infrequently – monthly or quarterly – or for only a small proportion of their scopes (such as focusing on duodenoscopes). This means that they have no idea whether cleaning is reliably effective during day-to-day operations.”
BENEDICT: “Olympus does not recommend/require cleaning verification testing as we have validated the cleaning process described in our IFUs. However, we support customers who choose to perform this optional step.”
EZAGUI: “Testing cleaning efficacy. Lack of facility policy to include ways to verify that the cleaning equipment used for processing of endoscopes is working.”
NEWTON: “Endoscopes are not always tested after each manual cleaning process. Endoscopes not meeting the FDA-required level of clean may not achieve maximum high-level disinfection or sterilization.”
AGOSTON: “The use of AERs is very good because the process is timed, standardized and recorded. Assuming that good manual pre-cleaning and cleaning procedures were followed, this is the state of the art for cleaning flexible endoscopes.
“Testing after manual cleaning is another important step. The weak link is in the technician’s skills and assurance that this is being done for every endoscope versus randomly. The goal is to have 100 percent assurance that every endoscope is thoroughly cleaned prior to sterilization or HLD. Those that perform random tests are not accounting for variation in the length of time that the endoscope was in use and exposed to bioburden, the pre-cleaning process or the time from the end of the procedures to the start of the cleaning process. All of these factors have an impact on how much and how affixed debris is. To randomly test for protein or ATP ignores these factors and places patients at risk. Testing should be done on every endoscope every time that it is manually cleaned.
“Some claim that disposable endoscopes are the solution. If we were to get to a positon were the cost of using a disposable versus reusable endoscope were equal or less then this would be a good idea for hospitals to convert. However, the total costs need to be included; those being acquisition (purchase and restocking), inventory tracking, repair, processing, disposal and any additional cost associated with the use of the device in the procedure room. The argument for or against disposable devices should be based on economics and safety only in the cases where the architecture of the device is found not to be safe for reprocessing (e.g., duodenoscopes). The reality is that if we cannot effectively reprocess flexible endoscopes, then we should look at all other devices with lumens and question our ability to reprocess these devices as well. The basic premise is that first the device has to be clean and then sterilized or HLD. If the device is not properly cleaned then efforts to sterilize or HLD will fall short.”
Cleaning verification testing - How to solve:
LORAN: “Endoscopes should be tested after each manual cleaning process to ensure they can be properly high-level disinfected or sterilized.”
WHELAN: “While further guidance and direction develops – through research, industry and standards – facilities should use an interdisciplinary team to discuss and determine the method and frequency of cleaning verification testing. This could include endoscopy, reprocessing, infection prevention and risk management. These decisions should be based on a careful review of available products, peer-reviewed literature, and should be in sync with whatever standards and guidelines the facility reprocessing policies are based on. Spelled out within those written policies would be the expected actions for failed results and repeat failures (despite re-cleaning). When choosing a cleaning verification process, it is important to identify the level of specificity desired as tests differ in this regard.”
FISHER: “There is no standard. This is considered a best practice, but not all facilities are conducting such testing. Make it the standard of care and require healthcare facilities to conduct random testing to verify cleaning.”
VANHEE: “Adenosine triphosphate (ATP) and protein testing offer great insights into the cleaning process for flexible endoscopes. However, without standardized methods and values for determining how ‘clean’ an endoscope is, it is difficult to determine the true value of the cleaning verification tests available on the market today. The key to cleaning verification using ATP, protein, or a combination of the two, as an indicator of cleaning efficacy is to determine baseline values of known contaminated and clean scopes at your facility to establish values for clean and dirty. These values can then be used to verify your cleaning process with a go/no-go threshold that must be met prior to starting the next step of the reprocessing cycle.”
KUBACH: “True culturing of high-risk models or specific endoscopes that may be related to suspected infections, requires quarantine of the item pending results. Failure to do so may release equipment prematurely with high concern microorganisms. Additionally, culture samples may be contaminated if great care is not taken during sample retrieval.
“A surveillance protocol should be established with staff. Training for proper sampling and how to handle an unfavorable result should be included.”
OFSTEAD: “Since scopes have to be clean for HLD or sterilization to work, I believe that cleaning verification tests should be done for every scope, every time. This is essential because the effectiveness of cleaning is not solely related to the effort and diligence of the reprocessing technician working in decontamination. We’ve learned that other factors may be as important, such as whether the endoscopic procedure was lengthy or particularly messy, whether the scope was adequately pre-cleaned at the point of care, whether there was a delay in transporting the scope for reprocessing, and whether there’s hidden damage inside the scope. The tech who’s working in decontamination may not know whether any of these other factors are in play, and as such they may go through the cleaning motions using good technique, not knowing that it didn’t work this time because of all those other things.
“Again, facilities should be providing cleaning verification materials and training for anyone who cleans endoscopes. When a test reveals that cleaning did not remove sufficient soil to pass the test, the techs and managers should approach the situation with curiosity, seeking to learn what factors may have contributed so they can reduce the incidence of failures and improve reprocessing effectiveness. Based on a high volume of inquiries related to cleaning verification testing, we developed a webinar that explains how to do the testing, what to expect and how to take action to improve outcomes based on the results.”
EZAGUI: “Testing equipment upon installing; during routine use (daily) and on all cycles used, after repairs and when changing to a new type of cleaning solution allows the user to verify process efficacy (IAHCSMM Endoscope, 2017, p. [Page 106]).”
NEWTON: “Endoscopes should be tested after each manual cleaning process. This provides immediate performance feedback to the cleaning technician and identifies endoscopes that need additional cleaning. A simple way to verify an endoscope is clean is to use an AER automated cleaning cycle that is validated for parametric release subject to successful cycle completion.”
GARRETT: “There are multiple commercial cleaning verification tests that exist such as ATP. These point-of-care tests provide an indicator of cleaning effectiveness but should not be used to evaluate an endoscope for cleanliness following high-level disinfection. There are many limitations to these tools, and users should carefully evaluate the existing commercial verification tools and use them an adjunct to existing facility auditing processes.”
AGOSTON: “Technician specialization and training are required to fix this weak link. The process of allowing every technician in an SPD to rotate and periodically process complex instruments like flexible endoscopes is a recipe for disaster. Repair costs will be higher and consistency of quality will vary greatly between technicians. In the GI department, this is less of a concern since the staff there typically only process flexible endoscopes and accessories.”
HLD and rinsing weak links
SPANOS: “HLD is not a reliable cleaning method, and this has been extensively documented in scientific literature. We take the position that the only acceptable incidence rate of contaminated scopes is zero.”
WHELAN: “A completely manual process of high-level disinfection (HLD) requires multiple human steps to ensure the endoscope is sufficiently exposed inside and out for complete disinfection. Any one step performed incorrectly risks inadequate protection for the patients to follow. Disinfectant solutions must be at the correct temperature and concentration, and the endoscope must be soaked for the correct amount of time to achieve full disinfection. Incomplete/inadequate water rinsing after disinfection risks exposing the next patient to harmful chemicals. Automated HLD processes decrease the human factor and offer more efficiencies and standardization; but automated processes can fail.
FISHER: “Pre-cleaning is the most overlooked; this is the second. When using any HLD, rinsing is the most critical step. By not rinsing thoroughly, you risk exposing patients to the harsh HLD chemicals during procedures. You also run the risk of chemical buildup making cleaning ineffective. Finally, if you terminal clean/sterilize the scopes at the end of the day, you run the risk of causing a reaction that can damage the integrity of the scope.”
VANHEE: “The high-level disinfection (HLD) process is an effective method of preparation of semi-critical medical device for patient use. Many flexible endoscopes fit squarely into the semi-critical Spaulding classification and HLD is an appropriate method. In general, high-level disinfectants can be classified into two discrete categories by the mechanism of action: Cross-linking vs. oxidation. Aldehyde-based chemistries, such as glutaraldehyde and ortho-phthalaldehyde (OPA), exhibit high-levels of cross-linking of proteins and amino acids that can lead to fixing of proteins to endoscope surfaces. On the other hand, oxidative chemistries, such as peracetic acid, do not require cross-linking as part of their microbiocidal action and have less risk of fixing proteins to the surface of the endoscope.”
KUBACH: “When manually high-level disinfecting it is important to make sure all air is removed, not just from the internal channels, but also from the exterior of the endoscope. Air bubbles that cling to the surface of the endoscope keep the disinfection chemical from getting good contact. Many manual flushing adapters should be removed to allow chemical contact as well or effective high-level disinfection will not be achieved. Strict adherence to temperature requirements should be monitored and documented.
“Areas that do not provide the required air exchanges should not be used and may cause employee injury.
“Manual rinsing requirements after high-level disinfection may be rather burdensome, often leading to partial completion. Certain chemicals may require three full water exchanges and three full channel rising steps. This may be made more likely to happen if using bins for rinsing that need to be carried, dumped, and refilled in a clean area. Remaining chemical residual can cause a myriad of complications if there is patient contact.
“MEC/MRC testing dwell and read time process is often not exact. If the strip is not handled and read at the designated read time, there is no reliable verification of chemical efficacy.”
OFSTEAD: “Attempting to disinfect dirty or damaged scopes [is one.] We’ve observed several breaches that reduce the effectiveness of the HLD process, including:
- “Using expired HLD
- Using expired HLD test strips (for MEC confirmation)
- Failing to test the MEC for each cycle
- Neglecting to maintain the proper temperature
- Inadequate exposure times
- Failing to flush channels with HLD
- Inadequate volume of rinse water
- Rinse water quality issues.”
DANIELS:
- “Failure to test disinfectant concentration: Disinfectant may no longer be effective
- Incomplete connection to AER: May not deliver disinfectant to internal channels
- Improper connectors: May limit flow to channels
- Contaminated rinse water: Water-borne contamination after HLD can create growth within the endoscope
- AER contamination: May re-contaminate endoscope during or after process.”
EZAGUI: “If the device is not rinsed adequately, the safety of the device may be compromised. Insufficient inventory levels leave technicians scrambling to place endoscope in AER too quickly, negating the rinsing process within manual cleaning phase.”
SARGENT: “HLD must first be understood. The nuances with each method are important in the understanding of the process and requirements to complete appropriately.”
AGOSTON: “The quality of the rinse water and how thoroughly the rinsing is done is most import for flexible endoscopes that are soaked versus those that are processed in an AER. The technician’s skills are the key to adequate soaking and rinsing.
Weak links in manual soaking are:
- Not completely submerging the endoscope in the HDL solution,
- Not flushing all lumens with HLD being sure that all air is removed from the lumens,
- Not soaking for the required time,
- Not testing the HLD to ensure that it is of the proper concentration/Ph./ temperature.
“The weak links in rinsing are:
- Not donning clean PPE prior to removing the endoscope from the solution,
- Not using critical water for the rinse and/or not rinsing per the IFU,
- Not flushing lumens with critical water per the IFU,
- Allowing the endoscope to contact dirty surfaces during or after the rinse.
- Facilities must ensure that critical water is available for the rinse.”
BAHOUT: “Major disadvantages of HLD include material incompatibility (e.g., peracetic acid, hydrogen peroxide) and human toxicity (e.g., glutaraldehyde) 2 and inadequate manual cleaning prior to disinfection.”
HLD and rinsing weak links - How to solve:
WHELAN: “Frequent monitoring of both manual and automated processes is required to ensure quality control. This should include monitoring for complete documentation of processes. Any automated process must be monitored and maintained per manufacturer IFUs. Review of and strict adherence to IFUs for endoscopes, chemicals, and equipment is necessary.
FISHER: “Education is a key to all these areas, especially cleaning. The IFUs and cleaning/reprocessing instructions have steps to follow. They need to be followed and not amended by the SPD staff to save time.”
VANHEE: “Although all FDA-cleared high-level disinfectants have proven microbiocidal activity, being aware of the different mechanisms of action of high-level disinfectants and their overall impact on flexible endoscopes, is critical to choosing the right high-level disinfectant for your facility.”
KUBACH: “Automation allows for standardization of required high-level disinfection steps and effective rising after disinfection. This also reduces risk associated with chemical contact and manual reprocessing errors. Automation should be considered. Training upon hire and continuing education for chemical requirements, use conditions, exposure risks and disposal regulations should be conducted annually.”
OFSTEAD: “Automating as many of the steps as possible; keeping meticulous documentation that is checked frequently; unannounced audits; and confirmation of adherence by checking HLD temperature, dates on water filters, HLD jugs and MEC test strip bottles, counting up the number of MEC test strips used and comparing it with the number of cycles.”
DANIELS: “Use a test strip to check a concentration of a detergent, focus on meticulous attention to detail ahead of AER, use AER to ensure consistency of process and change water filters on a regular and documented basis.”
EZAGUI: “The microbial quality of the water used to rinse endoscopes processed with LCS/HLD solutions is an important aspect in the sterilization or HLD process. Users should follow the recommendations of the device manufacturer and the LCS/HLD solution manufacturer for the microbial quality of the water to be used for rinsing (IAHCSMM Endoscope, 2017, p. [Page 130]).”
AGOSTON: “Allow only technicians who are specialist in processing flexible endoscope to perform the process. Ensure that all required accessories, water and supplies are available. In addition, I suggest moving to AERs whenever possible to avoid the above challenges of manual soaking.”
BAHOUT: “Users of any HLD should be thoroughly familiar with the product’s Material Safety Data Sheets (MSDS) and also ensure that it’s readily accessible for review. Users should also keep current with developments in products and practice, and be aware of advantages and disadvantages of the HLD that will potentially be used.
“It is impossible to disinfect an inadequately cleaned instrument. Any disinfection process is doomed to fail if cleaning is inadequate.3 Therefore the most important step in endoscope reprocessing is bedside flushing, with subsequent manual cleaning and brushing of endoscope channels.4”
Sterilization and aeration weak links
SPANOS: “Currently the data on successful sterilization is preliminary. However, we welcome a requirement for full sterilization of scopes. Transitioning from sterilization to HLD will likely require redesign of scopes to withstand the process. The design of the scopes as well as biofilm accumulation may prevent reliable sterilization, and further studies will be necessary to determine this. We feel a contamination rate of zero is the only acceptable number.”
WHELAN: “Not all flexible endoscopes are validated for all methods of sterilization. Not adhering to this risks damage to the endoscope. The material composition of flexible endoscopes does not allow for conventional methods, such as steam sterilization. Flexible endoscopes undergoing ethylene oxide sterilization require certain caps to be on or off (as per IFU) to allow effective aeration and prevent endoscope damage.”
FISHER: “As a manufacturer, we find that when customers mix modalities, it can be problematic. This is mostly due to the reaction of the different chemicals used in sterilization. The manufacturer must meet FDA standards, and this area is very important. A second issue deals with the manufacturers of the sterilization devices and their requirements for products to be placed in their sterilizers. With plasma, the products need to be dry for the sterilization to occur; whereas with steam, this is not a requirement. Customers now are forced to be creative in drying the product. This has led to an increase in damages to flexible endoscopes due to overheating caused by placing the scopes in an autoclave or drying tower.”
VANHEE: “Sterilization of flexible endoscopes is becoming an increasingly important and relevant topic in the present and future state of sterile processing. With more healthcare associated outbreaks linked to flexible endoscopes than any other medical device, the push toward terminal sterilization of some or all flexible endoscopes is stronger than ever. The challenge in the industry today is the lack of viable sterilization modalities for flexible endoscopes. Scopes with multiple, long channels, or other complex designs, such as colonoscopes and duodenoscopes, are not compatible with hydrogen peroxide gas and ozone low temperature sterilization modalities and ethylene oxide (EtO) gas sterilization requires a 9-18 hour full cycle time including exposure and aeration.”
KUBACH: “After manual cleaning, there is a tendency within some Sterile Processing departments to wipe down or soak the endoscope with low-level disinfectant chemicals to allow for bare handling in the clean area. Unapproved chemicals may cause damage to endoscope materials, components and epoxies. There is also no validation as to what residual of this chemical may remain within the materials potentially exposing the patient and there is no documentation as to how this chemical reacts with the approved sterilization method. Items that are not able to be run in the washer disinfection cycle should be considered and handled as contaminated.
“Hands down the most common mistake made during sterilization, as it relates to flexible endoscopes, is the lack of installing the venting cap. This will at the least result in over inflation of the bending rubber, and at the worst will cause the bending rubber to blow. The distal end may be damaged and other components such as fiber optic bundles and lenses may also be affected.”
OFSTEAD: “Attempting to sterilize dirty or damaged scopes, using unapproved trays or packaging systems, forgetting to attach the vent cap, attempting to sterilize wet scopes.”
BENEDICT: “Using incompatible sterilization methods for your endoscope. Sterilizing flexible endoscopes (or any other medical device) using a sterilization method that is incompatible may cause physical damage to the device, or may not have proven microbiological effectiveness.”
EZAGUI: “Many people believe that if an item is placed into a sterilizer and a cycle is run, the item will be sterile upon cycle completion. Nothing could be further from the truth! There is a lack of consistent training through the entire reprocessing cycle amongst technicians.”
SARGENT: “Education and time will allow for the understanding and importance of completing these steps each and every time a scope is processed.”
AGOSTON: “For Sterrad sterilization of small diameter flexible endoscopes, drying the flexible endoscope thoroughly prior to the process is very important to avoid aborted loads.”
DYBEC (NYU Winthrop/Ruhof): “Many older flexible endoscopes can only go through HLD and not be truly sterilized. Scope manufacturers are improving the capabilities of scopes and validating new sterilization methods. Hospitals and Endoscopy units must utilize available modalities.
Sterilization and aeration - How to solve:
WHELAN: “The endoscope IFU should be the first reference point for deciding whether your methods for sterilization are compatible. It is important to realize that different generations of a similar endoscope brand may have differing methods of sterilization validated.”
VANHEE: “Continued innovation in flexible endoscope design, materials and advances in low-temperature sterilization modalities are needed to make terminal sterilization of all flexible endoscopes a practical solution for sterile processing departments.”
KUBACH: “Documentation tying the patient to the serial number and the sterilization load is still often overlooked and misunderstood. Every endoscope that is used on a patient must be recorded and further the sterilizer run that addresses the rendering of that patient’s biological material as destroyed through sterilization must be recorded the same as if it were run in an AER. If there is an adverse event or infection, this record is required for traceability.”
OFSTEAD: “Collaborate with manufacturers to ensure that proper equipment and processes are used, train and retrain everyone involved, and automate the drying process to ensure all moisture is removed prior to packaging.”
BENEDICT: “Check with the manufacturer of your endoscope and sterilizer to ensure material compatibility and microbiological efficacy.”
EZAGUI: “A successful sterilization process requires meticulous preparation (cleaning, inspection, assembly, positioning, packaging and loading) and a functioning sterilizer. Everyone involved in the process must perform their role according to the manufacturer’s IFU, industry standards and guidelines and the known science of sterilization (IAHCSMM Endoscope, 2017, p. [Page 142]).”
GARRETT: “Currently, flexible endoscopes are classified as Semi-Critical devices under the Spaulding Classification and require High-Level Disinfection. Some devices are capable of undergoing sterilization but require an extensive aeration in order for the device to be rendered safe to use. Continued device development is needed to evaluate the long-term success of aggressive sterilization methods on flexible endoscopes, but in the meantime, several new, FDA-cleared flexible endoscope devices with sterile and disposable components have received 510K clearance and are available for users to reduce the infection transmission risk associated with ERCP procedures. “
AGOSTON: “Drying cabinets are very helpful in drying the endoscope.”
DYBEC (NYU Winthrop/Ruhof): “Upgrade to newer scopes that have been validated for current sterilization messages or upgrade to newer methods of sterilization to accommodate current scopes.”
Drying weak links
SPANOS: “We know drying is an issue with scopes, and the longer they retain moisture the more likely they are to develop bacterial CFUs. Additionally, specialty cabinets specifically designed for scope drying represent a significant capital cost outlay to hospitals. Even with drying cabinets, scopes are still shown to be contaminated.”
LORAN: “Drying is one of the keys to safe endoscope storage. Sufficient time, space and equipment play essential roles in achieving a dry endoscope.”
SWEENEY: “Several recent studies have brought to light a problem that had long gone unrecognized. Hanging scopes vertically in a cabinet does not remove all of the moisture from the channels. The surface tension of the micro water droplets is greater than the force of gravity. These droplets will remain indefinitely unless forced air is applied to cause evaporation.
“The air supplied must be instrument air and not just HEPA filtered (3 micron) air. The forced air should not become a source of contamination of the scope. It is also critical to monitor the line pressure in the scopes to ensure the scopes are not over pressured risking damage to the scope.
“Drying channels is now not only required for scopes in storage but also in for scopes used during the day going directly into use from the AER.”
WHELAN: “Incomplete drying of flexible endoscopes allows for development and proliferation of harmful biofilm and bacteria. This has been proven through research. Residual fluid has been directly seen in borescope examinations of endoscope channels. Mistakenly, staff often rely solely on Automated Endoscope Reprocessors (AERs) for drying, but AERs do not completely dry an endoscope. Additionally, many facilities do not have dedicated drying options factored into their physical operations. Current best practice for endoscope reprocessing calls for use of pressurized filtered forced air drying.”
FISHER: “Drying has become even more important with gas plasma sterilization. Customers are finding ways to creatively dry the product. Unfortunately, this has led to damage due to overheating the endoscopes. This can damage the epoxies and internal functioning of the endoscopes. Also, while alcohol is recommended for lumens, wiping the exterior of the scope with alcohol can dry out and affect the integrity of the bending rubber and shaft. Another area I have seen issues with is drying towers. Many have settings of ‘low’ to ‘high’ and not an actual temperature setting. This can lead to the endoscopes being exposed to higher temperatures than indicated in the IFUs.”
VANHEE: “As little as five years ago, endoscope drying was a rarely discussed step in the reprocessing cycle. Since then, it has become a significant area of interest for researchers, sterile processing professionals, and vendors alike. Retained moisture in flexible endoscopes promotes microbial growth and aids in microbial biofilm formation and removal of moisture in all endoscope channels and on the exterior surface of the endoscope significantly reduces the risk for microbial growth.”
KUBACH: “Many facilities have no reasonable means of extended drying and are commonly just externally wiping down and hanging in vented cabinets. Many do not even have access to wall air to initially blow out the channels. It may take days for internal channels to dry depending on the conditions. It has been shown that endoscopes that remain wet encourage microbial growth. Much attention has been raised to show that endoscopes and their related channels are very difficult to dry.”
OFSTEAD: “Relying on alcohol flush and air purge cycles in the AER to dry scopes, which doesn’t work; hanging wet scopes in the storage cabinets and hoping they’ll drip dry; using dirty towels to wipe down exterior surfaces; using a quick blast from an air pistol to evacuate the channels, which could damage the scope and does not remove all of the retained fluid; and using the same connectors and air pressure for all scopes.”
DANIELS: “Incomplete or hurried process fails to ensure complete drying and may leave residual water in ports. Incomplete drying [means] water provides hospitable environment for live contaminants to grow and creates an environment for biofilm formation.”
EZAGUI: “Inadequate drying of endoscope channels is a possible cause of replication and survival of remaining pathogens during storage. The presence during storage of potentially contaminated water in endoscope channels may promote bacterial proliferation and biofilm formation. An incomplete drying procedure or lack of drying and not storing in a vertical position are the most usual problems identified during drying and endoscope storage. Inadequate drying and storage procedures, together with inadequate cleaning and disinfection, are the most important sources of endoscope contamination and post-endoscopic infection ("Endoscope Drying," 2017).”
GARRETT: “Drying is critically important in reducing overall endoscope contamination but also the risk for biofilm transmission.”
SARGENT: Lack of knowledge or equipment – staff is either unaware of the importance of drying as well as the time parameters for drying in a cabinet or with air.”
AGOSTON: “The weak link here is allowing moisture to remain on or in the lumens of the flexible endoscope. Moisture is needed for the formation of biofilms.”
Drying weak links - How to solve:
LORAN: “Studies indicate all endoscope channels should be dried for a minimum of 10 minutes. Facilities should have sufficient endoscope inventory to support a 10-minute dry time before or during storage. An automated drying process saves valuable time and is more efficient than manual drying. “
SWEENEY: “Cabinet manufacturers have added channel drying to new cabinet purchases addressing these issues for both vertically and horizontally stored scopes. For facilities lacking the budgetary funds to purchase new cabinets there are inexpensive free-standing units available that will dry the channels during the day and prior to cabinet storage. Manual hand drying the scope, using instrument air supplied from the endoscopy unit, is also an option but can be very labor intensive. Each of the channel pathways must be dried for a minimum for 10 minutes and proper PSI settings must be in place to ensure there is no damage to the scope.”
WHELAN: “It’s Imperative to a review of current state is referencing against current standards, guidelines, and published research. Adding supplemental drying options designed and validated for endoscope channel drying enhances the ability to more effectively dry, especially interior channels for flexible endoscopes. Having the ability to test/measure for residual fluid allows for more objective assessment of drying adequacy. These test methods include borescope examination of endoscope channels and moisture indicators.”
FISHER: “Understand where alcohol is to be used and where it is not. Also, make sure that you are using approved drying techniques and not improvising.”
VANHEE: “Endoscopes must be dried completely, with highly purified air, prior to storage to maintain the level of disinfection achieved through the high-level disinfection process.”
KUBACH: “Extended internal drying is becoming the standard and can be achieved in multiple ways from drying boxes, current cabinet retrofits, and new cabinets that are able to connect and monitor drying time.”
OFSTEAD:
- “Use a clean, lint-free towel to dry the outside of each scope.
- Use one of two automated methods for drying channels: A drying station on the clean side with connectors for each type of scope and pressure-regulated instrument air that can be hooked up for automated drying lasting at least 10 minutes per scope Special drying cabinets that have hookups that circulate filtered air through all channels and around the external surface.
- Conduct drying verification tests on a routine basis to ensure the drying protocols are effective. Look inside ports and channels with a borescope. Use a chemical indicator to determine if there’s retained moisture.”
DANIELS: “Wipe down external surfaces before hanging. Follow manufacturer’s IFU for drying time, volume, pressure through channels. Manually dry the endoscope lumens with filtered pressurized air for an extended period of time after high-level disinfection and before storage in a conventional endoscope storage cabinet. Place the reprocessed endoscopes directly into a drying cabinet.”
EZAGUI: “Flexible endoscopes may be dried in automated endoscope reprocessors (AERs), manually, or in drying/storage cabinets. Flushing of the endoscope channels with 70 percent-90 percent ethyl or isopropyl alcohol followed by forced air drying is recommended by several guidelines. Current guidelines recommend that flexible endoscopes are stored in a vertical position in a closed, ventilated cupboard. Drying and storage cabinets have a drying system that circulates and forces the dry filtered air through the endoscope channels ("Endoscope Drying," 2017).”
GARRETT: “There are both manual and automated drying methods, but the most critical step here is to fully dry the endoscope which could take 10 minutes or more depending upon local environmental factors such as temperature and relative humidity.”
SARGENT: “Education and appropriate drying cabinets are essential to ensuring this step is completed without the possibility of contamination.“
AGOSTON: “Thoroughly dry the endoscope and force air of the proper pressure and or isopropyl alcohol through the lumens following instructions in the IFU. When hanging the endoscope, be sure that the umbilical and shaft hang straight down so that the technician is assured that there was no water in the lumens after the drying process. Also the use of hanging cabinets that have filtered and circulated air are a great idea. Lastly, access to the processed endoscopes should be limited and when prior to handling or touching the endoscopes clean gloves must be donned.”
Storage and handling (includes labeling and tracking) weak links
SPANOS: “Compliance represents a significant weak point here as it is dependent on no human error with labeling and tracking. As we know, scopes are often taken and improperly labeled or tracked. This problem is often exacerbated during nights and weekends. Cost is another barrier to this problem as we know tracking software represents a significant cost, ultimately driving up the per-use cost of reusable scopes.”
LORAN: “Storage and handling are key infection control points. Endoscope cabinets and transport trays can contaminate endoscopes prior to the procedure. Cabinet air type and pressure, materials and design can influence disinfection integrity. Transport trays can be difficult to clean or have the perception of clean. Residual bacteria can easily be transferred to another surface, staff, endoscope and patient.”
SWEENEY: “When using reusable transport containers proper labeling surface disinfection can become an issue. When transporting a clean scope, there can be no visible biohazard labeling on the container. If that same container is used to return the soiled scope, it must then have a biohazard label. Using dedicated clean and dirty trays will help with this but also creates significant storage and logistics problems. Clean trays must also be manually surface disinfected prior to each use. This can be very labor intensive and space restrictive.”
WHELAN: “Inadequate/improper storage and handling can negate all the work done to properly clean and disinfect flexible endoscopes. Recontamination occurs when endoscopes encounter unclean hands or surfaces. Flexible endoscopes stored horizontally may be at risk due to residual moisture. Flexible scopes coiled too tightly can damage internal components.”
FISHER: “While customers invest a lot of money in these endoscopes, very little is invested in the care of them. Having the correct tray or container is critical to protect these medical devices. Where HLD is used and the scopes are stored in a hanging cabinet, there are so many options. The gold standard is for temperature-controlled and constant-airflow. This can be very cost prohibitive. As for labeling and tracking, there are still facilities with no digital tracking that use colored tape to identify their product.”
VANHEE: “It wasn’t too long ago that flexible endoscopes were commonly stored in the open air by means of a hanger on the wall of the procedure room, storage closet, or reprocessing suite. Thankfully these storage means are becoming less common by the day as we continue to refine our endoscope reprocessing recommendations, guidelines, and standards. Proper storage and handling of flexible endoscopes is integral to maintaining the level of disinfection achieved through effective point-of-use cleaning, leak testing, manual cleaning, inspection, high-level disinfection (or sterilization), and drying.”
KUBACH: “Standard horizontal hanging cabinets are not made to accommodate all models and endoscope sizes. Double hanging is not allowed and endoscopes light guide tubes that contain channels cannot be looped without trapping moisture within the channels. Endoscopes need to fit the cabinet being used and insertion tubes should not touch the sides or the bottom of the cabinet. Poorly sized or overcrowded cabinets can encourage recontamination and impact damage.
“Cabinets may be made of materials that are porous and do not allow for effective cleaning or disinfection. Clean cabinet conditions are a must to maintain clean endoscopes.
“Endoscopes should have a visual cue that identifies it as clean. This discourages confusion once the endoscope is removed from the storage cabinet and reduces the risk that a contaminated scope may be reused by mistake. Using a tag dated with the last reprocessing date that must be removed to use the endoscopes greatly reduces this risk. There are also cabinets, RFID tracking programs and endoscope tracking software that will monitor how endoscopes are moved in and out of storage, when they are clean, and where they are located, further supporting traceability.
“Endoscopes storage does not always reside in the best location such as cabinets or shelves located with the procedure room. Moving high-level disinfected endoscopes in and out of the procedural environment greatly raises the risk of recontamination. Storage of sterile endoscopes needs to be maintained in the same conditions of normal sterile storage for temperature, humidity, air exchanges and facility policy for expiration.”
OFSTEAD:
- “Not consistently labeling scopes with reprocessing date
- Storing endoscopes in the procedure room
- Inadequate ventilation and failure to change air filters (if they exist)
- Not regularly cleaning and disinfecting cabinets (often because staff are not clear who is responsible — EVS, SPD, unit staff, etc.)
- Failing to use clean or sterile transport bins to protect patient-ready scopes during transport
- Exposing scopes to soil and pathogens by repeatedly touching them with bare hands when looking through the cabinets to select and transport scopes.”
DANIELS:
- :Transportation without protection provides opportunity for damage during movement and exposure to environmental contamination
- Transportation and storage without tracking may lead to ’borrowed’ equipment and loss of visibility of storage time and environment
- Storage in inappropriate cabinets [means a] lack of airflow may create environment
- Storage outside of appropriate cabinets allows environmental contamination and exposure to transient damage
- Inconsistent cabinet decontamination [means the] cabinet may become source of contamination.”
EZAGUI: “Inadequate storage and handling leads to contamination post high-level disinfection. Aging departments and tight financial budgetary constraints leave them to utilize existing cabinetry.”
GARRETT: “Healthcare facilities are responsible for maintaining their fleet of flexible endoscopes, and also tracking manufacturer loaner devices as well.”
AGOSTON: “Clean gloves should be donned when handling the endoscopes post-HLD and the endoscope should be transported in a clean and secure container to protect it from harm. Labels must be attached to clearly identify the endoscope and the date and information around when and by whom it was last processed.”
Storage and handling - How to solve:
LORAN: “Utilize endoscope storage cabinets constructed of non-porous materials that are easily wipeable. Cabinets should produce positive pressure HEPA-filtered air that prevents backflow of dirty air into the cabinets when doors are open and especially if vents are located on floor of the cabinet. Removable drip trays make it easy to clean the bottom of the cabinet. Look for cabinets with drip trays that remove when the door is closed or at least do not touch the distal end of the scopes when removed.
“Tray transport is equally as important to endoscope storage. If you utilize trays with lips or surfaces that are hard to clean especially where gloves make contact during transport, test those tray areas with an ATP device to ensure a clean surface. Disposable trays with porous surfaces should also be examined for cleanliness as anything that contacts the endoscope and staff could transfer bacteria. Sterile protective liners can be used to protect the endoscope and staff. Ensure the liners cover hard to clean and disinfect areas of the tray. Utilize transport trays that are easy to clean and disinfect and cart washer compatible for best infection control.”
SWEENEY: “Disposable trays with reversible lids provide the proper protection needed for the scope and easily transforms from a clean scope to a dirty scope by reversing the lid. As a linear process the space needed to store trays is greatly reduced.
“For reusable trays there are ‘clean’ labels available that peel back to expose a ‘biohazard’ label. This allows the same container to be used for both clean and dirty scopes provided they are properly disinfected each cycle.”
WHELAN: “All storage post-HLD needs to be dedicated, clean, dry, well-protected, and well-aerated. Endoscope accessories (e.g. buttons and valves) must be removed and stored with that endoscope. Conventional cabinet storage is in a dedicated clean area (not within the procedure room or reprocessing room), and allows scopes to be freely vertical hanging and protected from dust and debris. Dedicated endoscope drying cabinets (both vertical and horizontal) exist that allow continuous filtered forced air circulating through the cabinet, as well as through the endoscope channels. Once again, attention needs to be paid to IFUs from endoscope as well as cabinet manufacturers.”
FISHER: “Every endoscope should have the proper container for sterilization or storage.”
VANHEE: “Endoscope storage solutions should include a clean, secure, temperature and humidity-controlled environment that reduces the chances of cross-contamination. Emerging technologies in endoscope storage meet all the requirements for endoscope storage while incorporating endoscope drying cycles that circulate highly purified air through endoscope channels and around the exterior of the scope to maintain a dry, contaminant free environment for storing flexible endoscopes.”
KUBACH: “When choosing a cabinet confirm the materials are safe for chemical disinfection and make sure the cabinet will fit a space that is in an area in an acceptable location and under required storage conditions. Include visual cue tags or external tracking protocol in storage and transport procedures. Maintain documentation for humidity, temperature conditions, and cabinet cleaning schedules. Keep the bottom of the cabinet clear of all towels, chux, or associated supplies that may become wet from dripping and wipe out any moisture from the bottom of the cabinet.”
OFSTEAD: “One solution would be to sterilize all scopes and store them in wrapped trays so they will remain safe for patient use during storage and transport. If HLD is used, scopes should be stored in actively ventilated cabinets in areas with secure access. Scopes should be transported in closed containers that prevent contamination and damage. Staff and clinicians should be prohibited from touching scopes with bare hands to protect themselves and patients.”
DANIELS: “Use covered, rigid protection for transportation. Use a HEPA-filtered cabinet, at a minimum, to help prevent environmental contamination. Consider use of drying cabinets during endoscope storage. Consider additional protection for the distal end of the endoscope.”
EZAGUI: “When handling endoscopes, technicians must be aware of how microorganisms can impact the device’s safety. Prior to reprocessing, endoscopes must be handled in a manner that minimizes the risk of an endoscope cross contaminating the environment around it. This is accomplished by using a directional workflow, proper signage and containment devices, and by properly wearing personal protective equipment (PPE) (IAHCSMM Endoscope, 2017, p. [Page 164]).”
GARRETT: “Facilities should enter the endoscope serial number into the Electronic Health Record and maintain logs to improve traceability of the devices thru the reprocessing process and also patient usage information that is necessary in case of device recall or patient exposure situations. There are many systems such as tags, automated logs, and also instrument tracking systems that are commercially available to help healthcare facilities meet this need.”
AGOSTON: “Technician training is the key to success.”
Maintenance and repair weak links
SPANOS: “Scopes break routinely, and I doubt this is an item of contention. This represents a significant cost to a hospital system whether they utilize a repair contract or pay-per-breakage model. An addition problem with maintenance and repair is actual recognition of the repair need. Again, multiple peer-reviewed articles have determined that scopes in use had multiple abnormalities and breakages which had not been identified. The non-critical breakages degrade the performance of the scope while also increasing the probability the scope will retain pathogens.”
LORAN: “Maintenance knowledge and sufficient space to perform full inspections are often limited. Use of non-OEM or unqualified ISOs can reduce quality and increase overall costs and downtime.”
WHELAN: “Investigations and experience have shown that the older an endoscope is, the more likely damage exists and with that – risk. Damaged exterior surfaces allow access for bacteria and biofilm. Damage can result in parts of endoscopes becoming detached within patients. Within institutions, the monitoring for and identification of damage may be ineffectively performed and/or communicated (see inspection). To complicate things further, sequestering scopes for repair may not be within the sole control of reprocessing. Additionally, any/all reprocessing equipment may or may not be on a reliable schedule for preventative maintenance and repair.”
FISHER: “Customers partnering with an independent service provider to repair their critical medical devices and not partnering with the OEM in an attempt to save money.”
VANHEE: “Maintenance and repair are essential processes in endoscope ownership and use. Flexible endoscopes are a significant investment for any healthcare facility and proactive maintenance and repair can protect that investment and reduce the overall cost of ownership of endoscopes in general.”
KUBACH: “Endoscopes requiring repair are not always pulled in a timely manner. This greatly increases the chance of malfunction during patient use and the need for multiple endoscopes to complete the same procedure. There is generally not a clear understanding of preventative maintenance and most repairs are handled on a reactive maintenance basis. This can stress inventory needs and put the patient outcome at risk.
“Shipping transportation to repair facilities is often delayed and packing conditions may cause additional damage to delicate equipment.
“Upon return from repair, endoscopes are not always undergoing a complete receiving inspection and testing which may result in shipping damaged equipment or faulty repaired items to be placed back into service.”
OFSTEAD: “The biggest problem is that there are no standards, nor manufacturer IFUs for preventive maintenance for most scopes, and many facilities do not ensure that every scope undergoes routine PM. In many cases, scopes are not sent in for assessment or repair until they fail a leak test, cause complaints by the endoscopist, or have a catastrophic failure during a patient procedure. There are no rewards for identifying defective scopes that should be repaired, even though this protects patients, providers, institutions and manufacturers who could be held liable if patients are injured or infected. Technicians are commonly told to contain costs by ignoring minor defects and rationing their requests for repair.”
BENEDICT:
- “Perform procedures without first inspecting the endoscope or conducting a leak test. An endoscope in need of repair may harbor residual foreign materials and pose an infection control risk.
- Utilize repairs and/or modification by a third-party. The reprocessing instructions that you have been following from the manufacturer are no longer valid. Automated endoscope reprocessor manufacturers may not guarantee effective cleaning and disinfection. Reprocessing validation becomes the responsibility of the end-user.”
EZAGUI: “Quality management measures to track and reduce repair [means a] lack of preventive maintenance inspection programs.”
SARGENT: “Each step listed above leads to this step. If the scope is not leak tested, verified for cleaning, dried and handled appropriately, it may miss necessary maintenance or require maintenance due to mishandling.”
AGOSTON: “The weak link is the current standards and regulations not requiring notification of the physician when a flexible endoscope is found to have a leak post procedure. Hopefully, this will be changed as AAMI is revising ST-91 to include this recommendation. Other standards organizations should follow suit. IFUs are clear that if the endoscope fails a leak test or has some other damage, it should be removed from use and returned to the OEM for repair.
Another weak link is in the quality of the repair. All vendors should be qualified carefully to ensure that all parts, components and processes meet those of the OEM.”
DYBEC (NYU Winthrop/Ruhof): “Repairs of scopes and maintenance contracts can be very expensive. As a result many institutions sit on repairs, thereby reducing the number of available scopes.”
Maintenance and repair - How to Solve:
LORAN: “Hospitals can benefit from an effective preventive maintenance program to maintain endoscope integrity, reduce major repair costs and increase uptime. Utilize OEMs and ISOs that use quality parts with strict quality control systems. Train staff to identify needed minor repairs before they become major and more costly repairs. Ask your OEM or ISO to train your staff and provide ample space to fully inspect the endoscope.”
WHELAN: “For any device or piece of equipment within a healthcare institution, well-defined processes need to be in place for identification, communication and documentation of need for repair or replacement. To sustain this work, adequate resources must exist to allow staff the means to achieve this quality control – manpower, time and equipment. Clear systems for tagging scopes and equipment in question is crucial to both risk and cost reduction.”
FISHER: “OEM should be the standard for all critical medical devices.”
VANHEE: “As with any effective maintenance and repair program, the key is to catch issues early. When damage is detected early, it is easier and more cost effective to remedy the problem and get the endoscope back into the use rotation.”
KUBACH: “Utilizing per use inspection to identify and remove damaged endoscopes or those exhibiting use related wear and tear will facilitate timely removal. This can benefit increased case completion, safety, and limit greater damage affecting repair cost. Facilities should develop preventative maintenance plans for annual inspection and clarify removal procedures, packing requirements, return inspection requirements/documentation and transportation expectations.”
OFSTEAD: “PMs should be done for every scope based on usage patterns, durability and risks based on procedural use and patient characteristics. There need to be incentives for identifying scopes in need of PM or repair. A qualified expert should evaluate the fleet of scopes frequently.”
BENEDICT: “Inspect the endoscope prior to a procedure according to manufacturers’ IFUs. Send endoscopes for annual preventative maintenance inspection as recommended by the OEM. Use the OEM for endoscope maintenance and repair”
EZAGUI: “Training according to the manufacturer’s written IFU on the design, function, care and potential failures of all endoscopes in inventory and of new models as they are added to inventory and competency verification of leak testing, inspection for cleanliness and damage, channel identification, utilization of cleaning chemistries, and accessories and articulation (IAHCSMM Endoscope, 2017, p. [Page 200]).”
GARRETT: “Healthcare facilities should utilize the OEM manufacturer for all device service to ensure original manufacturer validated parts are used for repairs. Additionally, OEM manufacturers are subject to FDA inspections, licensing and are required to adhere to a globally-accepted and inspected quality system. If healthcare facilities choose to utilize third-party vendors that do not adhere to the same quality processes that OEM manufacturers follow, there is a potential risk that the device is not being repaired according to the manufacturer’s specifications, and this can result in potential patient safety risk.”
SARGENT: “Review of the IFU, create a detailed cleaning checklist, determine a preventive maintenance schedule to prevent unnecessary patient safety issues.”
AGOSTON: “Standards and regulatory organizations recognizing the significant issues of leaking endoscopes and the risk they pose to patients. Standards should be changed to include physician notification and documentation. Facilities must do their due diligence to be certain that the repair vendor is qualified to perform the necessary repairs.”
DYBEC (NYU Winthrop/Ruhof): “The key to reducing costly repairs is in the care and handling of the scopes. Education is an important part of this. Preventive maintenance can also reduce the amount of repairs.”
REFERENCES:
1 Guideline at a Glance: Processing Flexible Endoscopes. AORN, AORN J. 2016 Dec;104(6):610-615.
2 Rutala WA, Weber DJ. Disinfection of endoscopes: review of new chemical sterilants used for high-level disinfection. Infect Control Hosp Epidemiol 1999;20:69-76.
3Donlan RM. Biofilms and device-associated infections. Emerg Infect Dis. 2001 Mar-Apr;7(2):277-81.
4Weber DJ, Rutala WA. Lessons from outbreaks associated with bronchoscopy. J Hosp Infect 2001;22:403-8
Scoping out viable SPD strategic solutions to increase quality performance
Demanding, receiving and following validated instructions for use (IFUs)
2019 average score: 1.9
2018 average score: 2.5
Thoroughly educating, training, vetting and certifying SPD staffers on proper and effective cleaning techniques
2019 average
score: 2.5
2018 average score: 1.5
Switching to endoscopes that contain disposable/single-use-only components that can be swapped out (if available)
2019 average
score: 4.1
2018 average score: n/a
Switching to disposable/single-use-only endoscopic devices for selected endoscopic procedures only (e.g., bronchoscopy, etc.)
2019 average score: 4.3
2018 average score: n/a
Comprehensively monitoring and tracking all steps in the process with sensors and video technology
2019 average score: 4.7
2018 average score: 3.4
Holding staffers accountable/responsible for endoscope cleaning “violations”
2019 average score: 4.8
2018 average score: 2.8
Switching to disposable/single-use-only endoscopic devices for all endoscopic procedures
2019 average score: 6.1
2018 average score: 4.8
To maintain quality productivity in sterile processing, Healthcare Purchasing News asked more than 15 sterile processing experts to rank the following five strategies (1 being the most important/influential; 7 being the least important/influential). Please note that HPN emphasizes these are strategies, some of which may not be available in the market … yet. This year HPN added two choices into the mix that more specifically defined the adoption and use of single-use-only endoscopic devices. Last year’s scores are included for comparison.
What’s noteworthy is that HPN recorded a new No.1 involving a heightened emphasis on manufacturers’ instructions-for-use (IFUs), but also a significant technology shift as well. Big Brother and the Bullwhip plunged against the option of disposable/single-use devices. However, respondents didn’t embrace a complete conversion to these devices. Instead, they favored their use for selected surgical procedures or the ability to swap out disposable/single-use components if such an option were available.
Observers were allowed to suggest other alternatives that they ranked. Here’s what they added.
“Leadership planning to ensure adequate reprocessing time.”
“Increase Cleaning Technician Compensation: Endoscope cleaning is a tough and thankless job. Technicians stand over a sink following detailed cleaning instructions for many hours at a time with pressure to turn endoscopes around as quickly as possible for the next procedure. Their job is very important in preparing endoscopes to be safely high-level disinfected or sterilized. The combination of training, certification and increased pay drive and improve performance and infection control. Increased pay is a major component.”
“Balancing managerial support, inventory needs, case scheduling, ample staffing and properly allocated turnover time with strong reprocessing technicians that are compensated equally to the responsibility and weight of their job.”
“It’s acceptable to measure staff performance and ensure it is up to par and all steps are being [performed] adequately. Constructive feedback should be given to help them improve.”
“Provide comprehensive education to all users about the patient safety and infection control aspects of medical device safety.”
Do you agree with any of these findings and opinions?
Drop us a line at [email protected].
About the Author
Rick Dana Barlow
Senior Editor
Rick Dana Barlow is Senior Editor for Healthcare Purchasing News, an Endeavor Business Media publication. He can be reached at [email protected].