In a hospital, ambulatory surgery center (ASC) or other healthcare facility, many take for granted the process by which clean, sterilized surgical instruments reach the hands of surgeons and other clinicians for use on a patient. Two very important elements of the process are the storage of instruments until they are needed, and the transport of instrument sets and trays from the Central Sterile/Sterile Processing Department (CS/SPD) to the procedural area and back again, both of which must be performed with safety and efficiency.
Take a team approach
While the operating room (OR) is essentially the customer of the CS/SPD, that doesn’t mean OR staff members hold no responsibility for the handling and transport of instruments. In reality, both the OR and CS/SPD teams must play a collaborative role in these processes in order for the healthcare facility to deliver safe, effective and efficient care to patients.
Troy Scroggins, Product Manager, Sterile Packaging for Aesculap, comments on the challenges CS/SPD and OR teams face with regards to timing (delivering instruments where they are needed when they are needed) and ensuring the clinicians have the right instruments in right/proper conditions.
“Factors that cause case delays include holes in sets, missing or incorrect instruments (lack of organization/optimization) and dull or broken general and specialty instruments,” said Scroggins. “The mishandling of instruments can also lead to higher repair costs. Standardizing on a single container brand that is durable and includes a variety of options to accommodate a broad range of instrument types can help address these issues.”
For those facilities wanting to improve the storage, transportation and containment of instruments, she recommends they establish a multidisciplinary team to determine the goals and define the available “real estate” in terms of storage space.
“Investing the time and energy into designing or redesigning the sterile storage space can be time consuming; however, the benefits of a well-planned, well-designed area cut down on the stress and tension, as well as the overall efficiencies,” said Lane. “The collaboration between the departments (CS/SPD and OR) when implementing changes results in a much stronger relationship with all involved taking ownership for the process and success.”
She offers the following advice to facilities when taking a team approach to CS/SPD department and sterile storage area redesign:
- Secure surgeon buy-in to “trim down” the number of instruments in their sets, while increasing inventories when needed.
- Secure C-suite buy-in for additional surgical set inventory, rigid containers and additional storage space when needed.
- Design adequate storage in CS/SPD and the OR, ensuring that all areas are labeled clearly and that the items are not placed too close together or stacked, which creates clutter and confusion.
- Have OR and CS/SPD stakeholders walk through the proposed modifications multiple times over a few months prior to setting them in stone to ensure that they will be able to achieve the goals they have outlined.
Space-saving storage practices
Hospitals and other healthcare facilities that were designed and built decades ago typically find themselves outgrowing the instrument storage spaces originally designed to support them, explains Dave Salus, Market Manager, Healthcare Division, InterMetro Industries Corporation.
“Budgets are tight, so building in/on new spaces is not always an option, and when it is there is never room for waste,” said Salus. “Storage solutions need to be flexible in design and configuration to deliver high density, protective storage.”
Salus says CS/SPDs must take steps to reduce wasted space above and beside stored packs; install shelves that are rugged enough to hold metal containers, yet delicate enough to eliminate rips and tears in packs; and select partitions that are movable to adjust to varying pack sizes.
“Storage design choices should be flexible to provide high density storage like in track systems, or space reclaiming configurations that can utilize [typically wasted] space, like above case carts or other equipment,” Salus added.
Keep separate for safety
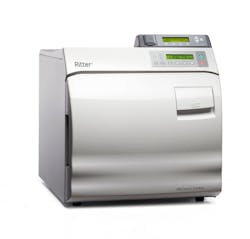
Darwin Asa, Marketing Manager, Midmark, stresses the importance of establishing and maintaining separate spaces for each CS/SPD function to boost efficiency and safety. He explains how department design can play a significant role in maintaining consistent and effective instrument processing practices that help safeguard the wellbeing of patients and staff.
“Additional attention should be given to ensure the size and layout of the instrument processing area fits the needs and workflow of the facility, allowing caregivers to treat patients effectively and efficiently,” Asa added. “The right design can help strengthen infection prevention programs and initiatives.”
Staying organized
Kevin Anderson, BSN, RN, CNOR, CSSM, CRCST, CHL, CIS, CER, Clinical Education Coordinator, Healthmark, says one way for CS/SPDs and ORs to improve instrument containment and transport is to simply organize their trays.
“We see this with vendor/loaner trays where items all have a specific spot within a tray,” said Anderson. “This makes it so much easier to see when an item is missing, or to find what you need. The same concept could be accomplished with many of our trays if we use simple tools like Secur-Its or other organizing tools within our trays. Having a streamlined design for our trays makes life easier for the end users in the OR, and for techs in SPD throughout the process. Organizing instruments within the tray may also improve the life of your expensive instrument assets.”
Turnaround times
Time is of the essence when it comes to the delivery of needed sterilization trays. The ONE TRAY Sealed Sterilization Container was cleared by the U.S. Food and Drug Administration (FDA) to be used to hold temperature-tolerant medical devices during steam sterilization cycles and then be stored up to 48 hours.
Barbara Ann Harmer, MHA, BSN, RN, Vice President of Clinical Services, IST, states that with the elimination of dry time when using ONE TRAY, the CS/SPD staff can react quickly to any changes or issues during the day’s schedule or address on-call situations when dealing with emergent needs.
“Add-on cases with insufficient instrumentation can now be scheduled knowing that a timely solution is available with the use of ONE TRAY,” said Harmer. “Torn wraps or other container systems that are found to be wet when needed are two other examples that are problematic for the timely delivery of sterilized trays. Late vendor trays, not a problem for ONE TRAY. ONE TRAY provides an efficient, economical and effective solution for CS/SPD daily concerns.”
Inventory Tracking
“Using technology, such as RFID, enables hospitals to benefit from a real-time inventory system that reduces delivery delays of critical items to avoid delaying or canceling surgeries, helps reduce labor costs in documenting used items and restocking any unused items, and shares information between departments or inter-network facilities,” said Kuehl. “RFID tracking also reduces overall inventory levels through knowing what is physically at the hospital, eliminates the hoarding of hard to get items for the OR, and tracks expiration dates, and in some cases, temperatures of critical items so only valid items are being used.”
Instrument tracking systems also protect patient safety by enabling these teams to track patient usage for infection prevention, and the number of reprocessing cycles to keep unusable instruments out of the hands of clinicians.
“CS/SPD professionals should pay close attention to the tracking and management of instruments coming in and out of the OR,” said Christopher John, Field Marketing Manager, Getinge. “By tracking which cases and patients these instruments are being used on, facilities can ensure that patient infection is kept to a minimum and tracking of trays and instruments have a full end-to-end documentation.”
“By using the T-DOC Sterile Supply Management Solution from Getinge to keep track of these trays/equipment, facilities can track usage and ensure that instruments in circulation are not being kept past their useful life, thereby keeping patients safer and staff happier by not using outdated equipment,” John added. “Tracking the movement of these instruments and trays helps keep track of units while they’re in use, dirty or being sterilized with estimated completion times.”
Protection during transport
As clean and sterilized instruments make their journey from the CS/SPD to the procedural area and back to the CS/SPD for reprocessing, there is always the risk for damage, particularly for delicate instruments that are not properly contained.
“Although there are many factors that contribute to the safe transportation of surgical instruments, instrument protection in the preparation and packaging area is a crucial component,” said Jamie Zarembinski, CCSPD, SPD Clinical Educator, Key Surgical. “Instrument protection not only provides an additional layer of safety for the end user of the instrument, but also protects instrumentation from damage during transportation.
“Surgical instruments often shift during handling and transportation of sterile instrument trays, which can cause damage to sharp and delicate instrument tips or compromise the sterile packaging integrity,” Zarembinski added. “Using a wide variety of instrument protection tools, such as tip caps and instrument sleeves, to protect surgical instruments from damage during transportation is a critical but an often-overlooked component of safe transportation of surgical instrumentation.”
Linda Condon, MBA, BS, RN, CRCST, Director of Clinical Services, Censis Technologies, explains how a stringer and tray liner are not always enough to protect instruments during transport because they can shift in the inner basket each time a container is handled.
Endoscopes in particular are vulnerable to damage during transport because of their delicate nature and high price tags, according to Aaron Lieberman, InstruSafe Product Group Manager, Summit Medical. He states:
“Organizing and protecting surgical instruments throughout the entire use cycle from decontamination, sterilization preparation, storage and transportation to the OR and back is what Summit Medical designs products for and the biggest areas of opportunity we see is the containment and storage of endoscopes. Taking care of your endoscopes can have a tremendous impact on your instrument repair and replacement budget.”
“Right now, we see a lot of rigid endoscopes, flexible endoscopes and robotic endoscopes being transported in plastic trays and metal baskets and these instruments are too delicate to be bouncing and sliding around during transportation resulting in expensive repair costs,” Lieberman added. “Using trays and transport containers that are specifically designed for each specific endoscope will protect them while they are most vulnerable, during transportation.”
Transport through public areas
“When surgeries come up unexpectedly and CS/SPD and OR staff members are trying to get instruments where they are needed in the heat of the moment, they quickly realize that their transport plans are unworkable, causing stress for everyone involved,” said Czarnowski.
Czarnowski explains that when that path of travel is blocked, disrupted or changed, the safety of patients, families and visitors may not be addressed, or may be overlooked. He says two common causes of disruption in the instrument transport path are construction and mechanical failure.
“As everyone who works in a hospital knows, construction is a constant fact of life,” said Czarnowski. “When hallways are blocked, new avenues for contaminated instruments must be found, or the instruments must be contained according to strict measures to protect the public.
Another instance is mechanical failure. The dedicated OR to SPD elevator is a common feature in hospitals. A contingency plan for when the elevator goes down must be made policy, trained for all roles involved, rehearsed regularly and enforced.”
When developing a transport path and plan, Czarnowski recommends that CS/SPD and clinical staff members take the time to test it out before implementing a policy.
“Come up with a potential plan and then have the people involved walk it and trial it on a low volume surgery day, for instance,” said Czarnowski. “Walk the path, see visitor areas, public areas, unrestricted areas and other areas you will encounter and adjust the plan from there before making it policy.”
Staff training
Even with all of the technologies on the market today to help improve instrument containment, storage and transport, perhaps the most critical element to success is CS/SPD and OR staff member training.
“Containers represent a significant expenditure for the hospital,” said Lawrence J. Slattery, Senior Consultant, Strategic Projects & Mobile Solutions, STERIS IMS. “This investment is intended to provide secure, sterile handling over time; however, container components are often mishandled and damaged resulting in questionable integrity. Whether wrapped or containerized, tray handling is critical. Instruments must arrive at the OR sterilized and ready for use.”
“Several hands touch the container components during the reprocessing cycle journey,” Slattery added. “Each touchpoint allows for mishandling, increasing the likelihood of holes in wrappers, which compromises sterility or allows possible content damage. Train staff on the importance of proper handling of trays and containers, and work to reduce touchpoints. Proactively maintain container components to ensure integrity.”
Custom tray pilot project eliminates ophthalmic instrument repairs
One instrument category that requires meticulous protection is ophthalmic instruments. Nuffield Health is the UK’s largest healthcare charity with 31 award-winning hospitals, 112 fitness and wellbeing clubs, healthcare clinics, and over 200 workplace wellbeing services.
Gordon Allan, Nuffield Health’s Hospitals Sterile Services Unit (HSSU) Surgical Instrumentation Manager, has been working on a project to reduce damage to fragile ophthalmic instruments through rationalization of sets and moving the instruments to custom Microwash instrument trays from Altomed.
“As an offsite sterile processing provider, our instrument sets are transported throughout the country and it’s therefore essential that we work to reduce the potential for damage to instruments in transit,” said Allan. “Not only do damaged instruments have a cost implication in terms of the repair/replacement budget, they also pose a significant risk to patients during surgery if not identified, increase turnaround time at SSD, reduce availability of sets and can ultimately increase the time a patient spends in surgery.”
Allan and his team implemented the Microwash instrument trays from Altomed in the health system’s Wolverhampton hospital at the end of 2019. This has resulted in a reduction in ophthalmic instrument repairs from 14 in 2019 (total cost £700, $910.69 U.S.) to zero in 2020. Based on these results they are projecting a saving of £3500 ($4,553.49 U.S.) over five years in repair costs alone.
About the Author
Kara Nadeau
Senior Contributing Editor
Kara Nadeau is Sterile Processing Editor for Healthcare Purchasing News.