Instrument preservation a full-time operation
For healthcare organizations, surgical devices and instrumentation have significant impacts on financial and clinical outcomes. There is the upfront financial investment to purchase these items, and the cost of ongoing maintenance and repairs. Having correctly functioning instruments available for patient cases enables the operating room (OR) to perform procedures and generate revenue, while lost, damaged or otherwise compromised instruments can result in case delays and potential patient harm.
The OR and the Central Sterile/Sterile Processing Department (CS/SPD) are the two key departments responsible for instrument preservation. Their actions directly impact instrument quality – and one another. Unfortunately, CS/SPD professionals often report that OR teams don’t always understand their role in instrument maintenance, believing that instrument care and cleaning is the sole responsibility of the CS/SPD. In these cases, when the OR neglects to perform the proper point-of-use cleaning, allows bioburden to dry on instruments and/or sends instruments to the CS/SPD in a disorganized manner, it increases the complexity and time of reprocessing, damages instruments and puts patients at risk.
On the other hand, when the OR takes the necessary steps to clean and care for instruments before, during and after use, instrument quality is maintained, reprocessing is streamlined and OR teams are more likely to have safe, effective and complete instrument sets available when they need them.
The OR can work together with CS/SPD to maintain and preserve surgical devices and instruments through open communication and collaboration through the initial prep, active use, cleaning and sterilization process.
Before the case
Before the surgeon has an instrument in his or her hand, there are steps the OR team can take in collaboration with the CS/SPD to support the preservation process.
Have what you need….
“Be well prepared for the case,” said Coss. “Have all your instrumentation available that you may possibly need for the case on the case cart. Instrumentation tends to become damaged when there is an urgency to get instrumentation to the OR. During emergent times, care and handling of instrumentation, by human nature, is not first priority.”
“The OR can help with instrument preservation before a case by ensuring they have the following: Enzymatic solution, sterile water, hard-sided container labeled ‘biohazard,’ and tags or locks for turnover of instruments/trays,” said Jones. “They should also perform an initial count/inspection of instruments per set according to the count sheet/recipe on the back table to ensure everything needed for the case is sterile and ready inside the room, test the functionality of scopes and cameras, and have repair locks or tags for broken instruments or those that need sharpening.”
…But only what you need
While it is critical for the OR to have what it needs up front in terms of instrumentation and supplies, it is also important that trays don’t contain unnecessary items. According to Michael Matthews, Director, Clinical Education and Training, Northfield Medical, recent studies have demonstrated that less than 20 percent of surgical instruments are used consistently in a single procedure.
“This means that as much as 80 percent volume of production in the Sterile Processing Department is waste,” said Matthews. “It is no surprise then, that most SPD technicians find it very difficult to give any instrument the time and attention necessary to ensure that it functions at the highest level of quality. Operating room personnel should partner with SPD and surgeons to streamline their instrument sets. Doing so will enable SPD to clean instruments more quickly, inspect instruments more thoroughly, as well as reduce the overall spend on maintenance and replacement.”
Kevin Anderson BSN, RN, CNOR, CSSM, CRCST, CHL, CIS, CER, Clinical Education Coordinator, Healthmark, recommends that the OR check case carts on the day of surgery to make sure that all the instruments they need are available and that extra instruments do not get opened by accident. This addresses any short-term issues related to unnecessary instrumentation, but in order to get to the root of the issue, OR teams must take a hard look at physician preference cards.
“The long-term way to help is to assist those in charge of preference cards to make sure that they are accurate and that instrument sets are optimized,” said Anderson. “That means, if instruments in the set are not being used consistently, then they should be removed and considered for peel pouch back-up stock.”
“This is termed tray optimization,” said Hadley. “Removing the underutilized instruments prevents over-processing and decreases processing time (due to a reduction of instruments on the tray). The instruments removed from the tray can then be packaged as single instruments or used to help build additional trays.”
“Powered by OpFlow technology, this process can take place using analytics driven by actual instrument usage data collected in the operating room,” Hadley added. “Being able to visualize instrument usage on a surgeon and procedure-specific level for a given tray enables you to reduce excess instrumentation and confidently implement optimized tray configuration changes.”
But what does an OR team do when they continue to find unnecessary instruments on trays regardless of physician preference cards’ updates? Just don’t open them up, says Seth Hendee, CRCST, CIS, CHL, CFER, CSPDT, CFER, Clinical Education Coordinator, Healthmark Industries.
“Extra instruments and/or sets may be added to a case for different reasons,” said Hendee. “For example, they are often there in case an instrument is dropped. Another reason for additional instruments is to accommodate for a potential change in the procedure, such as shifting from a laparoscopic case to an open. Not opening instruments that may not be used is a simple preservation step. While having extras on hand can be helpful, keeping them unopened until you are sure they will be used will save them from a processing cycle they did not need.”
Get organized
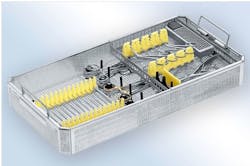
“Using instrument organization systems helps increase efficiency in the SPD by allowing staff to quickly identify and organize sets and identify any missing or misplaced instruments,” said Troy Scroggins, Sterile Packaging Product Manager for Aesculap. “In the OR, organized sets allow easy selection of the correct instrument and reduce surgical case time. It also extends instrument life by securing instruments so they are less likely to be damaged during processing and transportation. This translates to lower repair cost and higher set utilization. The higher rate of complete sets of better quality instruments delivered to the OR leads to improved relations between the OR and SPD.”
Perform a quality check
“The OR team members can make sure they are handling the instruments with the utmost care while checking for any contamination or the working ability,” she said. “It is important that the instrument be completely removed and checked before the case begins. This process requires that our OR team members are in the surgical case room before the patient and doctor arrive.”
During the case
While the patient on the table is the main priority of an OR team during a case, there are steps they can take to preserve instrument quality without detracting from patient safety or care.
Handle instruments carefully
Hendee points out that while stainless steel instruments are very strong and durable, they are not “bullet-proof.” Therefore, careful handling of the instruments by the OR team during a procedure will aid in preservation.
“Cutting edges, grasping jaws and other such delicate sections of instruments are prone to easy damage,” said Hendee. “Of particular concern are coated electrosurgical instruments. This coating is very easily damaged, and when that happens, it becomes a patient safety and OR personnel hazard. Leaks in electrosurgical instruments are known causes of patient burns and surgical fires.”
Clean at the point-of-use
As instruments and devices are used in a procedure, they encounter and can accumulate bioburden such as skin, flesh, blood and bone. Hendee explains how long-term exposure to this bioburden can damage instrumentation, stating:
“Patient soils are very harsh on instruments for two reasons. First, they affect the instrument’s surface and can cause rusting and pitting if left on for prolonged periods of time. Second, when soils are left to dry, they become very difficult to remove. This may require longer soaking or multiple reprocessing cycles to finally get all the soil removed, or worst of all, encourage someone to use incorrect tools to clean them. Wire brushes and scouring pads may remove the debris, but they will also cause damage to the instrument’s surface, which will cause or at least accelerate rusting and pitting.”
Point-of-use cleaning of surgical instrumentation is a well-known preservation practice, one that is recommended by the Association of periOperative Registered Nurses (AORN), the Association for the Advancement of Medical Instrumentation (AAMI) and the Association of Surgical Technologists (AST).
According to Greene-Golden, AORN section 3.2 to 3.3.2 describes guidelines for perioperative practice related to the care of instruments as they are used. She states:
“Point-of-use cleaning is the main goal for an OR team to help the sterile processing team in the preservation of the instruments used during the case. It requires the removal of gross soil and helps to stop the formation of biofilm. This process also helps the sterile processing team in their ability to clean the instruments without the worry of blood, organic material and debris that can cause corrosion, rusting and pitting. Failure of OR staff to perform point-of-use cleaning can make it challenging for CS/SPD staff to clean all of the instrument’s surfaces, thus reducing the efficacy of the subsequent sterilization process. If it is not clean it cannot be sterilized.”
When asked what steps the OR can take to help with instrument preservation during a case, Tim Cochran, Aesculap Technical Services Senior Marketing Manager, states:
“Instruments should be wiped as needed with a low or non-linting wipe and moistened with sterile water when possible during the procedure to remove gross soil (ie, blood and body fluids,) since these fluids are corrosive. Saline should not be used for pre-cleaning or keeping instruments moist because saline can cause damage when left on instruments for an extended period.”
“Instruments with lumens should be irrigated as needed throughout the surgical procedure to prevent obstruction due to organic material,” he adds. “Use sterile water for this when possible. Irrigation with sterile water maintains hydration of the bioburden on surgical instruments, which facilitates the cleaning of surgical instruments and prevents tissue damage.”“It (the sponge) can be dampened with sterile water and readily available for use from the surgical drape area or from the mayo stand to wipe off gross contamination during the case,” said Lewellyn. “A basin of sterile water can be further utilized once the case is complete. The technician can remove additional debris from lumens and other devices that may contain gross contamination, like bone from reamers used during orthopedic cases. Introducing this practice change to the interdisciplinary team is an approach to collectively assure uniform care for all surgical patients.”
As Hadley explains, it is not just the CS/SPD that benefits from point-of-use cleaning. Steps taken perioperatively to remove bioburden save the OR team time post-operatively as well.
“By keeping instruments clean perioperatively, the OR staff can significantly decrease the amount of time and effort it takes to decontaminate and clean instrumentation post-operatively,” said Hadley. “Some methods that the OR staff can employ include cleaning gross bioburden and body fluids from the surface, teeth and groves of instruments and flushing lumens regularly during the procedure using sterile water.”
Avoid damaging elements
“Some of the biggest enemies of surgical instruments are saline, eschar and rough handling,” said Michelle Lemmons, RN, BSN, Clinical Educator, OR, Key Surgical. “Intra-procedure point-of-use care should include: Only using the instruments for the purpose for which they were created, and only using sterile water to wipe/soak instruments and lumens. During electrosurgical cases, an anti-stick solution should be applied to the electrosurgical instrument prior to use to avoid eschar sticking.”
Matthews points out how stainless-steel instrumentation is protected from harmful elements by a nanometers-thin layer of a naturally forming compound called Chromium Oxide, which is what makes these instruments so resilient. However, Chromium Oxide breaks down with prolonged exposure to chloride-ions, which are found in blood, saline and disinfectant solutions such as Betadine.
“This is why point-of-use cleaning is so critical,” said Matthews. “If chloride-ions are allowed to sit on stainless steel instruments they will break down the layer of Chromium Oxide exposing the mostly-iron surface of the instrument to water. And as everyone who has ever accidently left one of their garden tools out in the rain knows, iron and water equal rust. With surgical instruments this takes the form of ‘pitting,’ which is essentially tiny holes in the instrument. Instruments with pits cannot be cleaned properly and are structurally unstable, making them unsuitable for use on patients. The loss of functional instruments is completely preventable through ensuring that instruments are wiped with sterile water during procedures, and blood is not allowed to dry on instrument surfaces.”
Experts agree that saline is a major threat to instrument preservation because it is caustic to stainless steel. Instead, OR teams should use sterile water for instrument pre-cleaning and take steps to ensure saline in not inadvertently used in place of sterile water in the OR.
“In many instances, when adding sterile water to the surgical field as a new practice, it may raise concerns for some team members and surgeons to have the water and saline near each other,” said Lewellyn. “The concern usually stems from getting them mixed up if the case is moving quickly. One solution to remedy this concern is for the team member scrubbing to have both sterile water and saline labeled either on the back table together or the sterile water separate from the back table on a sterile ring stand.”
After the case
The OR team’s responsibility for instrument preservation doesn’t end at the end of a case; rather it continues until the instruments are safely back in the CS/SPD for reprocessing.
Pretreat
While instruments should be promptly transported to decontamination following use so that the cleaning process can begin in timely manner, that is not always possible. When instruments sit and bioburden is left to dry on them, it makes it extremely difficult for CS/SPD staff to remove. Therefore, OR staff members must keep instruments moist and pretreat them with an enzymatic presoak solution to begin the decontamination process in the OR.
“To aid in the removal of blood soils in the CS/SPD, the OR can use a pre-treatment spray before instruments are sent to the CS/SPD,” said Ann Mangskau, an Assistant Marketing Manager with Ecolab Healthcare. “The pre-cleaner spray helps maintain moisture of the potentially corrosive blood soil, making it easier to remove during manual cleaning.”
“It is important to avoid the use of anything that may cause damage to instruments in your point-of-use pre-treatment process,” Mangskau added. “Saline, like blood soils, contains chlorides and is corrosive to stainless steel instruments and should not be used for instrument pre-treatment. Pre-cleaner sprays are formulated with components that are compatible with instrument materials, and products containing corrosion inhibitors provide additional instrument protection over those that do not.”
“Disassemble all multi-part instruments, spray enzymatic on the instrumentation to start the decontamination process or you can drape a wet towel over the instrumentation to keep the bioburden from hardening onto the surface,” said Coss.
Organize and protect
The way OR team members place instruments back into their trays is a major factor in protecting them from damage or loss. Jones recommends the following practices:
“The OR can help instrument preservation during a case by the following: Keeping all instruments opened and used with their respective surgical trays, open hinged instruments, disassemble multi-part instruments, separate reusable sharps, place heavy instruments on the bottom of the tray with lighter instruments on top, be very careful with the handling of scopes and cords (e.g. do not place any items on top of them), and tag and separate all malfunctioning/broken instruments.”
“Placing expensive cameras, rigid endoscopes, light cords, etc. in a way that minimizes the chance of damage is extremely important,” said Anderson. “I’ve seen these items come down to SPD all knotted up and just thrown into case carts haphazardly. These need to be sent down with the intention to prevent damage by placing them carefully back into protective containers.”
Transport with care
“Careful handling and transport of used instrumentation is an effective way to preserve them,” said Hendee. “Instruments that are hastily put into a transport bin or case cart are more likely to be damaged than those that are organized. When dealing with truly delicate instruments, separating and immobilizing them after the procedure, and then during transport, will reduce the chances of them becoming damaged greatly.
“Many delicate instruments are placed into specialty organizing containers,” Hendee added. “These containers may have silicone mats or holders to stop instruments from shifting and banging together during transport, whether they are clean or dirty. Replacing instruments into those organizers will help protect them in transport.”
Tips for getting OR on board
Knowing what is required of the OR and convincing the OR of the importance of performing these tasks are two entirely different matters. We asked our experts for tips on improving compliance with instrument preservation practices among OR staff members and they offered the following advice.
Show them the money
“Show them the department’s instrument repair bills - I am only kidding, well sort of,” said Hendee. “A large portion of an SPDs budget can be spent on instrument repairs. Instruments are a large investment, to begin with, and repairing them is a cheaper alternative to replacing them. Anything the OR can do to keep instruments out of the repair bin, which every SPD has, will help the department have funds to spend on other needs.”
“Secondly, I would also show them the department’s back table, and yes, every SPD has one of those too,” Hendee added. “It is not the same as an OR back table, however. This is where sets go when they are missing an instrument that is damaged or missing and is now awaiting replacement or repair. Especially with specialty or one-of-a-kind sets, having the set on the back table is a major issue and can cause case delays or cancellations.”
Find common ground
“SPDs must learn to communicate in ways that speak to the priorities of the OR, and vice-versa,” said Matthews. “Common ground that will appeal to both groups is the need for consistency, reliability and predictability. Each department must understand their part in ensuring that the instruments that are used on patients are safe and function as needed by the surgeon. SPD has an opportunity to become the expert on the tools that are being used by the OR staff. Equally, SPD must remain teachable about how the instruments are used during procedures so that they can better assess the functionality of the instruments. In short, both SPD and the OR have a responsibility to become experts on their own role while respecting the roles of their peers.”
Hold the OR accountable
“A policy pertaining to the process with strict enforcement of accountability is a great starting point,” said Lane. “When the OR and SPD have an open line of communication and dual ownership in the process on instrument handling, there is typically a lower incidence of instrument damage and comingling of sets. The process/buy-in from both sides can take some time to establish if it is lacking, so beginning with pictures and calling OR and SPD staff to come and look at the sets in question will typically get staff moving in the right direction. Staff knowing that they are going to be held accountable for instrument preservation is the quickest way to drive compliance.”
Jones recommends the CS/SPD implement the following practices to help communicate to the OR the importance of instrument preservation:
- A Six Sigma/Kaizen program that involves both the OR and CS/SPD working towards the same outlined goals.
- Allowing OR teams from each unit to rotate in CS/SPD for one month or a quarter in prep/pack; having them assemble the same sets they send to CS/SPD for reprocessing after their case.
- Require the OR and CS/SPD to develop a committee of stakeholders to meet weekly on instrument quality topics.
Collaborate and communicate
Hadley suggests that regular meetings between members of both departments can provide a forum for giving and receiving information.
“Don’t assume that OR staff know or understand the significance of proper instrument management,” said Hadley. “These meetings can provide training, education and information that leads to a collaborative partnership. Ultimately, the goal of collaboration is the development and implementation of sustainable processes that leads to effective instrument preservation.”
Educate and train
Cochran recommends educating OR team members on the importance of instrument preservation and what a lack of preservation could lead to, such as pitting and damaged instruments.
“Demonstrate how to properly handle the instruments or have your repair vendor hold a training class,” he said.
Cochran also advises the assessment of instrument and container quality on a regular basis to identify any changes that could be warning signs of larger issues, such as water quality or the need for preventative maintenance.
Anderson says while the CS/SPD can be involved in the education and training process of the OR, and device manufacturer representatives could also serve in the education capacity, the expectations should be set by CS/SPD and OR leadership. This kind of collaboration will help bridge even seemingly simple gaps, such as OR and CS/SPD using different names for the same instrument. These miscommunications lead to frustration and additional unneeded instrument handling and wear.
“It is important that these measures are valued not only by CS/SPD, but also by the OR leadership,” said Anderson. “Once expectations and education has been implemented, auditing for performance should be done and reported at regular intervals. Reporting on audit data could be done at team huddles or on quality metric bulletin boards on a weekly or monthly basis. This data could also be used for performance reviews of individuals as well.”