Lehigh Valley perioperative business team soars through surgical savings
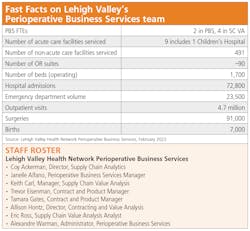
When it comes to helping surgical services holistically control expenses and generate cost savings in how they care for patients and equip clinicians across the sprawling Lehigh Valley Health Network in the eastern Pennsylvania, a small team of six certainly means business.
Led by Alexandre Warman, Administrator, the Perioperative Business Services (PBS) team specializes in perioperative services support, network perioperative value analysis and perioperative data analytics to enable surgeons, physicians and nurses to perform surgical and endoscopic procedures as cost-effectively as possible across 18 distinct locations. This team also manages centralized scheduling and billing for the Network.
Warman’s team reports to the President of Lehigh Valley-Hecktown Oaks and the Vice President, Perioperative Services. The second team, Contracting and Value Analysis, led by Allison Hontz, Director, reports to the Vice President, Supply Chain and Chief Procurement Officer.
“We are two teams in two different divisions, but attached to the hip,” Warman noted.
Roughly 90 miles due west of New York City and roughly 60 miles northwest of Philadelphia, Allentown may serve as the hub for Lehigh Valley’s network, but within the last four years the PBS team has seen its sphere of influence span coordinated health sites in nearby Bethlehem, Phillipsburg and Stroudsburg as well, with the number of surgical procedures supported exceeding 88,000 in fiscal year 2021 from nearly 56,000 four years earlier, a 57% growth rate in volume. And they’re projecting more than 91,000 in fiscal year 2022, according to Warman.
The expansion motivated Lehigh Valley to centralize and standardize processes for surgical and endoscopic procedures throughout the network, which helped to bolster enterprise-wide value analysis efforts.
The necessity to leverage market share and partnerships with key suppliers became necessary, Hontz and Warman explain to Healthcare Purchasing News. As LVHN acquired new facilities, the need to centralize and standardize became priority. From a Surgical Services perspective [value analysis] moved to a Business Service function and grew to cover all 18 locations, they emphasize.
Lehigh Valley created a Network Value Analysis Steering Committee in 2019 that oversaw seven committees specializing in selected areas, including radiology, patient care, surgical services, pharmacy, cardiology, business/purchased services and physician practice offices a k a LVPG (for Lehigh Valley Physicians Group).
In 2020, Lehigh Valley created the Network role of Director, Contracting and Value Analysis, and hired Hontz for the position. She reports to the Vice President and Chief Procurement Officer of Supply Chain but also has a connection to all seven of the Value Analysis Committees.
And while PBS may mean business, it’s not all business.
“I would say that it is not 100% a business function,” Warman said. “I think it is purely just under the name of business, but we are 100% a mix of both clinical and business, utilizing all members of the team.”
Rather than launch a value analysis project exploring a particular specialty, such as cardiology or orthopedics due to the high cost of implants and supplies and recruiting surgeons to participate based on outcomes-based data, PBS instead spread out more holistically across the enterprise, earning the team the inaugural Surgical Performance Excellence in Supply Chain Award by HPN.
“It doesn’t make sense to silo the work,” Warman said. “LVHN utilizes physician chiefs and physician leaders in addition to business leaders and other subject matter experts to lead projects. Other (Subject Matter Experts) SMEs include [Information Systems], Infection Control, Supply Chain Analytics, Supply Chain Management, Value Analysis (VA) and other VA teams as necessary, as there is overlap with many products. We collaborate as a team. It does not come from top down or bottom up, but rather from the collective group.”
Lehigh Valley wanted PBS to move away from the silo mentality several years ago as an impetus for the Network VA program.
There are many products, services and devices out there that intermingle with many divisions in healthcare, according to Hontz and Warman, so the steering committee meets monthly to discuss challenges, progress and next steps.
Quick wins, lasting results
Warman attributes data analytics and value analysis as integral components to PBS’ success.
“This team has designed and implemented innovative solutions [that] offer leadership readily available data to improve efficiency, lower cost and provide the highest quality patient care,” he noted. “The development of key performance dashboards has provided business intelligence around procedural volume, length of stay, and efficiency metrics such as, on-time-first-case-start percentages, turnover times, same-day cancellation rate and case scheduling accuracy. This team continues to push forward with innovation, linking surgical case data with quality and cost data. These efforts continue to set LVHN apart from health systems across the nation.”
At press time, with an operational blueprint in place and generating results, Lehigh Valley and PBS were exploring ways to automate this process through an enterprise resource planning (ERP) system as well as an automated electronic VA system, according to Hontz and Warman.
Achieving perpetual cost savings in surgical services can be challenging, Warman indicated.
“While LVHN has implemented quick wins with savings strategies, including reducing the number of vendors utilized across service lines, [such as] urology, orthopedics, and general surgery, LVHN has come up with ways to engage our front-line colleagues to find cost savings while keeping patient safety and quality a priority,” he said.
Hontz acknowledges that a series of quick wins can help establish credibility with clinicians, but the process extends much more deeply.
Even though items might seem [like] a quick win, such as a surgical blade conversion for better price, there is still a great amount of collaboration, education and work processes that must be followed, according to Hontz and Warman. They acknowledge that while monitoring the quick win, they still have to make sure that no other products are being brought in that are similar, and they continuously measure quality and outcomes through monthly VA meetings. Clinical feedback and integration are critical as they rely on the entire collaborative team – including physicians – so that the VA process is followed regardless of quick win or not, which drives the integrity of the process.
Pandemic posed challenges
Warman says he saw the COVID-19 pandemic as an opportunity for PBS that he did not want to go to waste.
“While we utilized COVID as an opportunity to review sustainability and purchasing power, we were limited to what we could actively achieve,” he said. “While LVHN did postpone inpatient volume in 2020, this was for a four-week period. By May our operating rooms were running at 125% to recover the postponed surgical volume.”
They approached contracting accordingly.
“Our Supply Chain actively sought contracts that would sustain and cover the increased volume despite strict supplier allocations and backorders,” Hontz indicated. “This was an achievement [in and] of itself. Lesson learned, our Supply Chain now incorporates new ideas and language when negotiating new contracts.”
It takes a team
Instead of recruiting a single person to spearhead this process and ride herd, Lehigh Valley dedicated a department to drive it.
Warman indicates that decision was by design.
“To be successful in VA you must understand the theory of constraints,” he said. “You are only as good as getting through the process of your weakest point. To achieve this, it takes a team. Active projects in Surgical Services are approximately 30, and there are an additional six VACs at LVHN.”
Hontz prefers to treat the VACs and clinicians as customers.
“We share and bring initiatives to each other as well as work together on analysis projects and implementations,” she added. “We must co-exist as everyone shares a responsibility in the project.”
PBS motivated teamwork and achievement using gamesmanship, according to Warman.
Throughout fiscal 2020 to date, PBS created multiple initiatives, such as the “Periop Olympics” and “Super Bowl of Savings,” to recruit nurses and VA teams to participate in cost-saving initiatives. Among the accomplishments: Supply reduction and PAR level reviews across operating rooms that delayed nearly $161,000 in operational purchases during a three-month period, he noted.
“This colleague engagement raised the interest of our surgeons which led them to begin their own campaign of cost reduction by removing the preference from their preference cards and moving to procedure-based cards,” he said.
Five notable quantitative examples include the following:
• TURP (transurethral resection of the prostate) averaged $577.00 a case, and was reduced to $450.00 a case for $5,461 in annual savings
• TURB (transurethral resection of bladder tumor) averaged $277.00 a case, and was reduced to $186.00 a case for $2,093 in annual savings
• PERC (pulmonary embolism rule-out criteria) averaged $1,443 a case, and was reduced to $1,016 a case for $5,124 in annual savings
• Lap chole (laparoscopic cholecystectomy) averaged $641.00 a case, and was reduced to $429 a case for $75,189 in annual savings
• Lap Appe (laparoscopic appendectomy) averaged $786.49 case, and was reduced to $747.60 a case for $22,284 in annual savings
Warman and Hontz add that they continue to explore further cost savings in fiscal 2022.
Cost-cutting infusion
PBS though Supply Chain Value Analysis emphasizes the Quadruple Aim principles daily, according to Warman.
“Our dashboard creation and surgical scheduling are examples of ‘Better Health and Better Care,’” he indicated. “Examples of ‘Better Cost’ can be found with our experienced charge posters and value analysis team. They provide daily audits to ensure the accuracy of our supply and implant usage in all cases. FY2021 case charge posting accuracy was over 95% for the entire team. Our team is recognized as an important and critical asset to our Perioperative Nursing, Anesthesia and Surgical colleagues across the health network.”
Through PBS’ efforts with clinicians and administrators, annual cost reductions ranged from more than $925,000 to more than $3.2 million during the span of a six-year period, 2015 to 2021, according to Warman. More than $2.5 million in savings was generated in FY2021 alone, he added. Since beginning these efforts, Lehigh Valley has booked more than $10 million in cumulative cost savings. Lehigh Valley participates the regional group purchasing organization AllSpire that works with HealthTrust as its national GPO.
“We continue to empower our front-line colleagues to find savings across the system,” he added.
In fact, Lehigh Valley builds the Quadruple Aim into its annual performance evaluations so that staffers are assessed on better care, lower costs and patient and employee satisfaction.
“Value Analysis is a systematic, objective, evidence-based process that brings together stakeholders having product and clinical use, knowledge, financial analysis and purchasing contracting expertise to reduce overall cost while maintaining or improving quality,” he noted. “We are making quality decisions and balancing the needs of multiple constituents in the healthcare delivery systems. In short, value analysis is the conduit to accomplishing the quadruple aim in today’s healthcare environment.
“LVHN performance evaluations allow our leaders to provide attainable goals that match LVHN corporate goals,” he continued. “Based on each goal achieved by the individual determines a final score.”
Warman’s and Hontz’s teams strive for clinical and operational integration, too. Although many definitions and explanations of clinical integration remain available throughout the industry, Lehigh Valley explains its own effort through a visual representation of a golden star [See figure 1], as well as through seven key tenets.
• Accountability comes from the entire team
• It does not come from top down or bottom up; it requires everyone to be on the same page
• Transparent data are shared in standard meetings
• Individual interventions are sent for outlier performers
• We enlist clinical leadership and physician champions in opportunity identification and communication across all initiatives
• All data is vetted with our VA team, surgeons, and Operating Leadership prior to presenting to all teams, which is critical to fostering colleague and surgeon trust
• We include all formulas, calculations and methodologies in presentations
Hontz and Warman expresses pride in their team’s accomplishments to date.
“The colleague engagement and experience provided by this team is endless, as observed by their achievements,” they agreed. “The daily efficiency, drive, pride and innovation of this team of incredibly enthusiastic colleagues supports LVHN’s mission to heal, comfort and care for the people of our community.”
Honorable Mention
McLeod Health
About the Author
Rick Dana Barlow
Senior Editor
Rick Dana Barlow is Senior Editor for Healthcare Purchasing News, an Endeavor Business Media publication. He can be reached at [email protected].