Proper endoscope cleaning requires visual cues — even for the invisible
Proper cleaning and verification of this process is paramount to achieving high-level disinfection or sterilization of flexible endoscopes. It is well known that if a device, especially a flexible endoscope, is not cleaned properly it may never be able to be adequately disinfected or sterilized.
Removal of soil and inspection of the device for residual debris or damage are critical steps in assessing the quality of reprocessing and whether the device is fit to move on in the process. Items that are deemed to be in disrepair should be taken out of service immediately and devices that show signs of having residual soil in or on them either by cleaning verification test or by visual inspection, should be re-cleaned and re-tested until they pass both the inspection and verification tests.
Generally speaking, the broad steps that encompass endoscope reprocessing are as follows:
- Pre-cleaning
- Leak testing
- Manual cleaning
- Rinse after cleaning
- Inspection (visual inspection and cleaning verification)
- High-level disinfection
- Rinse after high-level disinfection
- Drying
- Storage
Step No. 5 is a newer step in the process that many facilities may not be aware of. This step of inspection of endoscopes occurs after the manual cleaning process and prior to high-level disinfection or sterilization of the device. A visual inspection of the scope and cleaning verification test after cleaning are addressed in current flexible endoscopes reprocessing standards and guidelines including AAMI ST911, SGNA2, and AORN.3
Guidelines, recommendations
Visual inspection and verification can detect the presence of residual soil and identify items in need of repair. According to ANSI/AMI ST91, healthcare facilities should establish a comprehensive quality assurance and safety program to monitor all aspects of endoscope processing. This program should incorporate both visual inspection and testing of the equipment to identify conditions that may affect the cleaning or disinfecting processes. Visual inspection alone may not be sufficient for assessing the efficacy of the cleaning processes. Therefore, the use of methods that are able to detect organic residues that are not readily visible should be considered in facility cleaning policy and procedures.1
SGNA states that, “Visual inspection is usually included within manual cleaning and not listed as a separate step. However, due to the recent issues with reprocessing, visual inspection warrants its own step. It may be considered a “time out” or safety stop to verify that the endoscope is at least visually clean before proceeding to HLD. It follows the rule that an item must be cleaned prior to HLD, with all endoscope surfaces coming in contact with the disinfectant solution, to ensure that all organic material is removed.”2
According to the AORN endoscope reprocessing guideline section recommendation VII, “Flexible endoscopes, accessories, and associated equipment should be visually inspected for cleanliness, integrity, and function.” Furthermore, section XIII.f. states that, “Cleaning verification tests are used to verify the ability of the cleaning process to remove, or reduce to an acceptable level, the organic soil and microbial contamination that occurs during use of a reusable device. Cleaning verification tests include chemical reagent tests for detecting clinically relevant soils (e.g., protein, hemoglobin, carbohydrate) and ATP. Periodic verification of cleaning effectiveness may help reduce errors in manual cleaning and improve effectiveness.” Also, in section VII.c., “Lighted magnification should be used to inspect endoscopes and accessories for cleanliness and damage.12,13,65 [2: High Evidence] An endoscope that appears clean may harbor debris that cannot be seen without magnification. Lighted magnification may increase the ability to identify residual soil or damage.”3
Spotting evidence
What are the kinds of evidence you should look for before endoscopes proceed to high-level disinfection? According to the guidelines, the endoscope should be inspected visually for conditions that could affect the disinfection process such as cracks, corrosion, discoloration, retained debris, and poor fiber optic illumination.1 Other items to inspect for, as noted by AORN, are cleanliness, missing parts, clarity of lenses, integrity of seals and gaskets, moisture, physical or chemical damage, and function.3 The use of magnification and adequate lighting does help assist in the visual inspection process to identify these abnormalities.1 These are the common warning signs that the scope is in need of repair or additional processing.
Other warning signs that an item may not be ready to be disinfected or sterilized are peeling of adhesives, cracks in lenses, brush gouge/scrape marks at the distal tip, stretched out covers on the bending section, and soil around or under the control knobs. Essentially, compare the scope to a new one and identify what is different. Then, evaluate if this could be a significant issue that may impact the ability of the scope to be cleaned, disinfected, or sterilized and could this be a risk to the patient?
There are other more obscure warning signs that the endoscope may need more attention or that reprocessing procedures are not in a state of control. Things like moisture retained in the channel upon inspection with a borescope after disinfection would tell you that your drying processes are not adequate. Retained lint/fibers are also very commonly seen upon inspection with a borescope and would bring to light the possible practice that staff members are not using lint-free or low-linting clothes or sponges during reprocessing. Retained brush bristles would warrant investigating the condition of reusable brushes or the possible practice of reusing single-use brushes mistakenly. Internal channels that are heavily damaged by gouging or scraping may warrant taking a look at the physician practices with endoscope accessories, such as keeping the distal tip angulated while passing or removing a biopsy forceps.
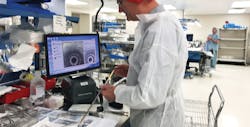
Use of a borescope for inspection of internal channels of the endoscopes is an additional step that may be taken to engineer quality into an endoscopes reprocessing program. Both ST911 and AORN endoscope guidelines3 do highlight the process within their document. For example, AORN states that “Internal channels of flexible endoscopes may be inspected using an endoscopic camera or borescope. [2: High Evidence] Endoscopic cameras and borescopes penetrate the lumen and allow for improved visual inspection.3
Certainly, inspection of the internal channels with a borescope is a quality-driven process and will help a facility to assess the condition of their endoscopes, the overall reprocessing procedures and potentially the drying process. The one issue that is often raised with inspection with borescopes is when to perform this process.
Many facilities inspect their scopes periodically after the disinfection process is complete and the scopes are in storage. If doing this, then the scope should be reprocessed again before use. By performing inspection at this stage in the process, a facility can assess their internal drying practices and clearly determine whether it is currently being performed adequately or not. According to SGNA, scopes must be completely dry prior to storage or should not be used on patients without being reprocessed again.2
Other facilities will inspect with a borescope after manual cleaning prior to disinfection or sterilization. Although this is an option, the scopes are highly contaminated at this point and completely wet internally. A complete drying procedure would need to be initiated after cleaning in order to inspect with the borescope. If not, all that will be seen is water, which is not helpful.
Therefore, to perform a visual inspection, at a minimum the unaided eye should be used to inspect the external surfaces of the endoscope after manual cleaning. Additionally, current standards and guidelines do call for the additional use of lighted magnification to be added to the process of visual inspection.1,2,3 The process of performing cleaning verification is also clearly warranted based upon the current standards and guidelines.1,2,3 Borescopic examination of internal channels is a newer process, but one that is recommended within AAMI ST911 and AORN endoscope guidelines.3
References:
- ANSI/AAMI ST91:2015, “Flexible and semi-rigid endoscope processing in health care facilities.”
- SGNA Standard of Infection Prevention in the Gastroenterology Setting, 2016: http://journals.lww.com/gastroenterologynursing/Citation/2016/11000/STANDARDS_OF_INFECTION_PREVENTION_IN_THE.9.aspx
- AORN GUIDELINE FOR PROCESSING FLEXIBLE ENDOSCOPES, Revised February 2016 for publication in Guidelines for Perioperative Practice, 2016 edition
Recap…