When it comes to monitoring patients, most clinicians would agree that they could use another set of eyes on the back of their heads and 10 more hands to do the job. Instead, caregivers are often tasked with having to do more with less.
“Our customers, particularly respiratory therapists and nurses on the general and medical-surgical floors, are being asked to manage more patients at once than ever before,” said Julia Strandberg, Vice President, General Manager, Medtronic Health Informatics & Monitoring. “With the expansion of continuous monitoring protocols and systems, clinicians have an abundance of patient data that they are supposed to address, interpret, and use to prioritize patient care. However, depending how monitoring systems are designed and implemented, many clinicians have said that they often have too much information to process and not the right tools to efficiently aggregate patient data. As a result, they may be overwhelmed by patient data and not able to use it as it is intended — to inform and improve patient care.”
Fortunately, new and innovative technologies are emerging at a steady pace to assist healthcare workers in making sure that brains, skin and every organ in between get the right care and attention — at the right time — so patients can heal faster and go home.
Vitally important
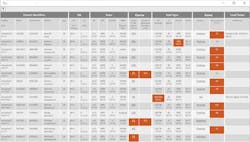
The customizable Medtronic Vital Sync Monitoring & Clinical Decision Support (CDS) solution was launched in May and has several modules designed to improve workflow and communication. The Vital Sync virtual patient monitoring platform gathers patient information that clinicians can access remotely via data analytics, CDS apps and reporting. This feature can be accessed on the spot using a web-enabled device. The Vital Sync physiological patch, also wireless, is a lightweight device applied to a patient’s sternum to continuously collect physiological data — heart rate, respiration rate, single-lead ECG and body position — which automatically transmits to the Vital Sync system. The Vital Sync Weaning Readiness and SBT Monitoring app allows clinicians to set weaning readiness criteria and alerts for mechanically ventilated patients. It remotely tracks the breath-by-breath progress of each patient through a spontaneous breathing trial, alerting clinicians whenever patients fall outside the predefined thresholds. The Vital Sync Early Warning Score app provides early warning scores that are based on automated calculations that will indicate if a patient is at risk of deterioration before it becomes critical.
“The first clinical warning signs of a Code blue can appear as early as 6 hours prior to an event; an Early Warning Score system that gathers data from multiple parameters can be highly valuable,” Strandberg said. “The criteria settings within our CDS apps are based on published, proven clinical protocols and based on a subscription model that is scalable — it can be deployed on a single floor or across an entire hospital system so they may scale up during flu season or other times of high patient traffic.”
Special-need patients
Caring for very overweight patients usually presents unique challenges. For example, obtaining an accurate blood pressure reading on obese patients, who are already at high risk for cardiovascular disease, renovascular disease, and other medical problems, can be tough to achieve.
“It is difficult to obtain accurate noninvasive blood pressure (NIBP) measurements on these patients because it is not possible to select a properly sized BP cuff,” explained Cory Stahl, Global Marketing Manager, Monitoring Solutions, GE Healthcare. “As a consequence, clinicians use upper arm cuffs to measure NIBP from the forearm, an application for which such cuffs are not clinically validated. Use of upper arm cuffs in this manner has been shown to underestimate systolic blood pressure by as much as 10 mmHg.”
GE’s CRITIKON RADIAL-CUF, the first clinically validated BP cuff, was introduced three years ago to be used exclusively on the forearms of obese patients. And since the disposable cuff (free of DEHP and natural rubber latex) remains with the same patient throughout his or her hospital stay, it provides an added way to help halt the spread of infection.
“Our study found a clinically significant difference in the accuracy of NIBP measurements between the CRITIKON RADIAL-CUF and the conventional upper arm cuff when both were used on the forearm,” Stahl added. “ In our study the upper arm cuff underestimated systolic blood pressure by almost 10 mmHg (mean error = -9.85 mmHg) compared to the value for the RADIAL-CUF (mean error= -0.12 mmHg ). Another measure of the accuracy of the cuff is the percentages of readings that are within 10 mmHg of the reference value. With the CRITIKON RADIAL-CUF, almost 90 percent of the systolic readings met that criteria, with the upper arm cuff only slightly more than half of the readings were within 10 mmHg.”
Moms and babies also have special needs that require careful monitoring and attention. In early May, PeriGen Inc., launched the PeriWatch HUB, a software module for labor and delivery units that allows caregivers to continuously prioritize patients based on abnormalities in vital signs, fetal heart rate and labor progression from an electronic dashboard. “With the HUB perinatal dashboard we aim to facilitate earlier identification of deteriorating patients. Since delayed response to critical conditions is the most common human error leading to adverse events, there is a strong clinical need for this application,” stated Matthew Sappern, Chief Executive Officer at PeriGen.
“At MedStar Health, Cues (the fetal monitoring pattern recognition module of HUB) has been found to help reduce NICU transfers and lower the need for fetal resuscitation by over 50 percent,” added Sappern. “Another system, this one in the Pacific Northwest, tells an anecdote of how the use of PeriWatch Curve, the labor progress module of HUB, helped them avoid doing a cesarean section for one of their patients.”
Preventing pressure injuries
Despite how preventable they are, hospital-acquired pressure ulcers (HAPUs), or pressure injuries, are all too common in the healthcare setting. Everyone knows that patients must be turned regularly in order to avoid pressure injuries. But getting it right isn’t easy — especially when relying on traditional methods.
“Most healthcare institutions depend on nurses to manually observe patients and intervene when needed to help prevent immobility-related conditions like pressure ulcers, pneumonia and patient deconditioning,” said Mark Smith, Vice President, Sales and Marketing, Leaf Healthcare. This labor-intensive approach to monitoring is time consuming, inefficient and often impossible for busy staff. What nurses tell us is that they want a patient monitoring system that automatically monitors and documents mobility and alerts them when necessary so they can more easily identify and focus on the patients who need the help.”
Enter the Leaf system, a wireless, award-winning patient monitoring tool that cues caregivers at the precise time when a patient needs to be repositioned to alleviate pressure from hi-risk areas. The single-use patient sensor is waterproof, weighs less than an ounce and operates on batteries that last three weeks. The disk is placed on the patient’s upper anterior torso to track and monitor body position 24/7 whether he or she is in bed, on a chair or walking. The data is constantly delivered to any web-enabled device with color-coded visuals and countdown timers to help clinicians quickly identify and prioritize patients who will need to be turned. The technology is also customizable to accommodate turning periods and angle, tilt angle and other protocols. It even notes when a patient self-turns and starts the clock over automatically — a unique feature that saves nurses significant time and energy by not having to make unnecessary trips to patient rooms.
“A presentation at the Symposium on Advanced Wound Care meeting last fall showed how one hospital intensive care unit cut their HAPU rate by more than 50 percent by using the Leaf sensor on critically ill patients, said Smith. “Even more dramatic results from a 1,200-plus patient, randomized controlled trial at a major academic research medical center are pending publication. Another hospital experienced a 79 percent reduction in expenditures for rental beds and specialty support surfaces when it began using Leaf to ensure patients were turned and repositioned more regularly.”
Stop the noise!
Today’s monitoring technology is improving and that certainly makes patient care easier and more effective to carry out but there is a hitch: alarm fatigue. Day in and day out clinicians get hit in the ears with dozens of alerts. It’s not surprising some become desensitized to the noise and when that happens, serious accidents can occur. Missed ventilator alarms, for example, is on ECRI Institute’s Top 10 Health Technology Hazards for 2017. False alarms are another problem that often occurs because parameters or thresholds were set improperly.
“A key challenge on the general care floor to nursing in regards to continuous monitoring is the significant impact of alarm communication, particularly as it relates to false alarms, on providing adequate coverage of patients,” said John Zaleski, PhD, CAP, CPHIMS, Chief Analytics Officer, Bernoulli. “Patient-to-nursing ratios in these environments can range from 5:1 up to 12:1, which means there is a significant workflow burden to nursing and adding to that burden by communicating alarms from devices that provide continuous monitoring could indeed increase risks and patient safety hazards rather than decrease them due to the constant potential for distraction.”
Bernoulli’s Respiratory Depression Safety Surveillance (RDSS) solution is designed to help reduce the problem. Launched in March, RDSS offers patented analytics with multi-variable thresholds that can be customized and measured continuously.
“The key to addressing false alarms is correlating events that, when taken individually, may not be actionable, But in combination, may be,” said Zaleski. “The RDSS platform provides connectivity to a hospital’s existing fleet of pulse oximeters and capnography from a wide range of vendors. It utilizes comprehensive real-time data to provide active patient monitoring, eliminating the exclusive reliance on individual device alarms to inform clinicians regarding the patient’s condition. RDSS also integrates with mobile clinical communication tools to deliver the right alarms and alerts to the right caregiver at the right time.”
Bernoulli recently collaborated with an East Coast hospital to conduct a study that is published in the Journal of Biomedical Instrumentation & Technology. The outcomes were notable. “Passing multiple series of data through a multi-variable rules engine that monitored the values of HR, RR, SPO2 and ETCO2 in order to determine which alarms to send to the nurse-call phone system brought the number of respiratory depression alerts down to 209—a 99 percent reduction,” said Zaleski. “More importantly, the RDSS analytics alerted for every patient that experienced an actual respiratory depression episode requiring intervention.”
Todd Plesko, Vice President of Product Strategy, Vocera Communications, adds a slightly different perspective.
“While alarm fatigue is a well-documented concern in healthcare, perhaps even more critical is interruption fatigue,” Plesko said. “Interruption fatigue occurs when care team members are distracted by alarms, alerts, and notifications as well as text messages, phone calls, overhead pages, etc. All of these distractions and interruptions add to clinicians’ already heavy cognitive load. In addition to taking time away from direct patient care, constant interruptions can cause critical alarms to actually be missed or ignored, causing a patient safety issue. “
The Vocera alarm management solution manages alerts, alarms and notifications from more than 120 clinical systems, text messages and voice calls from a single platform. Once the facility’s clinical protocols are programmed into the Vocera Platform, it begins to filter actionable vs. non-actionable events, prioritizing them and sending alerts only to the appointed or available clinician via his/her preferred communication device.
“Clinicians can easily distinguish between alarms from multiple sources and different priorities based on the audio and visual information sent directly to their device of choice — whether it’s an iOS device, Android, Blackberry, laptop or workstation,” Plesko said. “The Vocera Platform acts like an air traffic controller, managing all the interruptions to help ensure smooth workflows. Real-time information and notifications such as early warning sepsis alerts, critical lab alerts, and patient vitals enables care teams to respond quickly and appropriately. All alarm events and responses are date- and time-stamped and logged in real time, providing robust data and an audit trail to identify potential gaps in communication and processes. Analytics from the solution help hospital leaders better understand alarm trends per bed, unit, staff, alarm type, alarm density, distribution and response times.”
With only 16 percent of frontline nurses satisfied with the current alarm management system at Sentara Princess Anne Hospital in Southern Virginia Beach, the facility decided to implement the Vocera platform. The results were noteworthy. “Data showed a 54 percent reduction in secondary NICU alarms within 30 days of integrating the alarm management technology with the RTLS system,” Plesko said. “Prior to integrating the Vocera system with the RTLS, NICU nurses said they experienced alarm fatigue 95 percent of the time while on shift. After implementation, this same nurse population said they experienced alarm fatigue less than 16 percent of the time during their shift.”
The EarlySense contact-free monitoring system is another way to continuously monitor and better manage alarms — and it requires no leads, sensors or cables.
“The sensor is placed under the bed mattress and wirelessly and continuously monitors heart rate, respiratory rate and motion,” said Tim O’Malley, President, EarlySense. “This makes it very comfortable for the patient, while also providing health teams with accurate, real-time data and collecting thousands of valuable readings over a four-hour rounding period. With the EarlySense system, the alarm frequency in a typical eight-hour shift can be as low as two to three alarms. In comparison, other devices, such as telemetry and oximetry, can generate hundreds of alarms per shift.”
Newton-Wellesely Hospital in MA implemented an Early Detection initiative which included the EarlySense system and saw a 59 percent reduction in alarm response time. Additionally, according to research sponsored by EarlySense and published in the American Journal of Medicine EarlySense’s continuous monitoring system was found to decrease code blue events by 86 percent, reduce patient falls by 43 percent, and reduce pressure ulcers by 64 percent. It also helped decrease total length of stay and ICU transfers.
Finding ways to communicate effectively with today’s swelling patient population in ways that will increase understanding and promote behavioral changes is also an important focus.
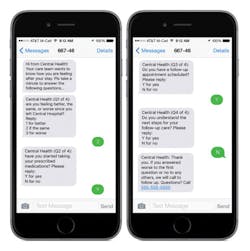
“As reimbursements continue to decline and the need to more fully engage patients increases, budgets don’t exist to ‘throw people at the problem,’” said Kenneth Saitow, President and CEO, CareWire. “Today’s traditional communication channels – paperwork, phone calls, emails, and patient portals – are becoming less and less useful in the healthcare context. Healthcare consumers have come to expect more convenient and timely means of communication, and there is a need to reach as many patients as possible, regardless of socio-economic status and age, not to mention primary language spoken.”
CareWire’s technology is a HIPAA-compliant mobile solution that helps clinicians engage and activate patients across the continuum of care by educating and motivating them to adhere to their care plans while simultaneously keeping doctors and nurses up-to-date with each patient’s health status.
“All interactions begin with a text message, an application that virtually everyone has on their phone and uses regularly,” said Saitow. “Links within text messages serve as a gateway to the mobile web where patient portals, self-service capabilities, and multi-media education is easily and quickly accessed. We support a HIPAA-secure messaging channel for the safe and secure exchange of protected health information. We also include provider personnel tools to monitor and respond to interactions in real-time, which is key to integrating the solution into day-to-day workflow.”
Saitow said the technology is expanding to include socio-economic and behavioral predictive analytics coupled with a patient’s activation history (an “activation index”) to support more precise and customized messaging, calls to action, and follow-up.
About the Author

Valerie J. Dimond
Managing Editor
Valerie J. Dimond was previously Managing Editor of Healthcare Purchasing News.