CDC awards $117 million to advance innovation and health equity in federal initiative to end HIV
CDC awarded $117 million to state and local health departments to help rebuild and begin to expand HIV prevention and treatment efforts as the U.S. continues to respond to COVID-19. The awards are part of the federal Ending the HIV Epidemic in the U.S. (EHE) initiative, which funds 57 priority areas to expand and tailor key HIV prevention strategies to community needs.
This is the second major round of CDC funding delivered to state and local health departments as part of the initiative and builds upon initial investments. The funds will be used to expand access to the initiative’s four major strategies and to reduce health disparities. Total awards range from $1.9 million to $10.6 million. CDC distributed the available funding based on the burden of the epidemic and the number of focus counties within each state.
Outreach will be expanded and strengthened in key settings critical to reaching people at risk for HIV who may not otherwise have access to healthcare services. These efforts will expand syringe services programs (SSPs) and invest more in sexually transmitted disease specialty clinics.
Racial, ethnic, and geographic disparities have contributed to HIV prevention gaps for far too long. EHE is working to address these disparities and achieve health equity through a comprehensive approach that focuses on providing resources where they are needed the most, and meeting people where they are with the services they need. This includes acknowledging the root causes that contribute to these disparities — such as poverty, unequal access to health care, limited education and employment opportunities, systemic racism, homophobia, stigma and discrimination — and working to implement policies, practices, and programs that help overcome these obstacles.
EHE works by scaling up four key strategies: Diagnose, Treat, Prevent and Respond. This includes expanding innovations in testing and care delivery spurred by COVID-19, including telehealth and self-testing, as well as same-day delivery of testing and pre-exposure prophylaxis (PrEP) and treatment. By providing testing and care services in more accessible, convenient ways, these innovations will address long-standing barriers to prevention and care.
While communities have already begun expanding these activities, a significant increase in resources is required to deliver many innovations and programmatic activities at the level needed to meet the initiative’s goals. The FY22 President’s Budget requested $275 million, $100 million increase above FY21 for CDC’s EHE efforts. CDC will continue to work with communities to expand these high-impact HIV diagnosis, treatment, prevention, and response strategies.
Innovative, community-driven solutions are at the heart of EHE and are already showing what is possible with expanded investment, collaboration, and locally tailored strategies. Recipients have developed plans for how they will use these and other funds to carry out each of the initiative’s four key strategies to meet local needs. For example:
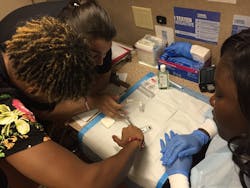
- Diagnose: Over 80% of jurisdictions plan to promote and increase access to HIV self-tests, and conduct testing via mobile testing units and/or in non-traditional settings including churches.
- Treat: Over 60% of jurisdictions will expand telemedicine services that allow patients to access medical services remotely, especially in rural areas, and rapidly engage in care and start treatment within seven days of diagnosis.
- Prevent: Over 70% of jurisdictions will start or expand programs to connect people to PrEP services and establish or expand SSPs, where legally permissible, using innovative delivery options such as mobile testing units and peer-delivery systems.
- Respond: At least half of the jurisdictions will develop plans to respond to HIV outbreaks by establishing a dedicated workforce and improving the use of real-time information to direct resources to the communities that need them most.
Recognizing the important role that community-based organizations (CBOs) have played and will continue to play in providing these and other critical HIV prevention and care services to people that have or are at risk for HIV, CDC requires that at least one-quarter of recipient funding go to activities implemented by CBOs. CDC is planning to award an additional $9 million later this year to support at least 60 front-line CBOs to develop self-testing programs and distribute self-test kits in these communities.